Electrocardiography is the process of producing an electrocardiogram, a recording of the heart's electrical activity through repeated cardiac cycles. It is an electrogram of the heart which is a graph of voltage versus time of the electrical activity of the heart using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including:

Ventricular fibrillation is an abnormal heart rhythm in which the ventricles of the heart quiver. It is due to disorganized electrical activity. Ventricular fibrillation results in cardiac arrest with loss of consciousness and no pulse. This is followed by sudden cardiac death in the absence of treatment. Ventricular fibrillation is initially found in about 10% of people with cardiac arrest.

A premature ventricular contraction (PVC) is a common event where the heartbeat is initiated by Purkinje fibers in the ventricles rather than by the sinoatrial node. PVCs may cause no symptoms or may be perceived as a "skipped beat" or felt as palpitations in the chest. PVCs do not usually pose any danger.

Wolff–Parkinson–White syndrome (WPWS) is a disorder due to a specific type of problem with the electrical system of the heart involving an accessory pathway able to conduct electrical current between the atria and the ventricles, thus bypassing the atrioventricular node. About 60% of people with the electrical problem developed symptoms, which may include an abnormally fast heartbeat, palpitations, shortness of breath, lightheadedness, or syncope. Rarely, cardiac arrest may occur. The most common type of irregular heartbeat that occurs is known as paroxysmal supraventricular tachycardia.

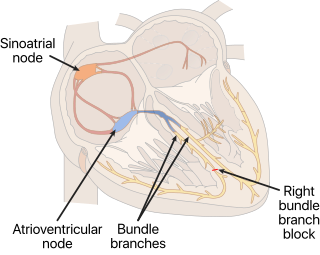
The bundle of His (BH) or His bundle (HB) ( "hiss") is a collection of heart muscle cells specialized for electrical conduction. As part of the electrical conduction system of the heart, it transmits the electrical impulses from the atrioventricular node to the point of the apex of the fascicular branches via the bundle branches. The fascicular branches then lead to the Purkinje fibers, which provide electrical conduction to the ventricles, causing the cardiac muscle of the ventricles to contract at a paced interval.

Third-degree atrioventricular block is a medical condition in which the electrical impulse generated in the sinoatrial node in the atrium of the heart can not propagate to the ventricles.

The cardiac conduction system transmits the signals generated by the sinoatrial node – the heart's pacemaker, to cause the heart muscle to contract, and pump blood through the body's circulatory system. The pacemaking signal travels through the right atrium to the atrioventricular node, along the bundle of His, and through the bundle branches to Purkinje fibers in the walls of the ventricles. The Purkinje fibers transmit the signals more rapidly to stimulate contraction of the ventricles.

Ventricular tachycardia is a cardiovascular disorder in which fast heart rate occurs in the ventricles of the heart. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple episodes over a short period of time are referred to as an electrical storm. Short periods may occur without symptoms, or present with lightheadedness, palpitations, shortness of breath, chest pain, and decreased level of consciousness. Ventricular tachycardia may lead to coma and persistent vegetative state due to lack of blood and oxygen to the brain. Ventricular tachycardia may result in ventricular fibrillation (VF) and turn into cardiac arrest. This conversion of the VT into VF is called the degeneration of the VT. It is found initially in about 7% of people in cardiac arrest.

AV-nodal reentrant tachycardia (AVNRT) is a type of abnormal fast heart rhythm. It is a type of supraventricular tachycardia (SVT), meaning that it originates from a location within the heart above the bundle of His. AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia. It is more common in women than men. The main symptom is palpitations. Treatment may be with specific physical maneuvers, medications, or, rarely, synchronized cardioversion. Frequent attacks may require radiofrequency ablation, in which the abnormally conducting tissue in the heart is destroyed.

In electrocardiography, the T wave represents the repolarization of the ventricles. The interval from the beginning of the QRS complex to the apex of the T wave is referred to as the absolute refractory period. The last half of the T wave is referred to as the relative refractory period or vulnerable period. The T wave contains more information than the QT interval. The T wave can be described by its symmetry, skewness, slope of ascending and descending limbs, amplitude and subintervals like the Tpeak–Tend interval.

A bundle branch block is a partial or complete interruption in the flow of electrical impulses in either of the bundle branches of the heart's electrical system.

The QRS complex is the combination of three of the graphical deflections seen on a typical electrocardiogram. It is usually the central and most visually obvious part of the tracing. It corresponds to the depolarization of the right and left ventricles of the heart and contraction of the large ventricular muscles.
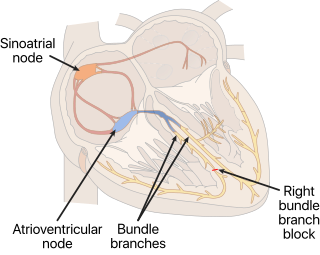
A right bundle branch block (RBBB) is a heart block in the right bundle branch of the electrical conduction system.

Left bundle branch block (LBBB) is a conduction abnormality in the heart that can be seen on an electrocardiogram (ECG). In this condition, activation of the left ventricle of the heart is delayed, which causes the left ventricle to contract later than the right ventricle.
In cardiology, an accessory pathway is an additional electrical connection between two parts of the heart. These pathways can lead to abnormal heart rhythms (arrhythmias) associated with symptoms of palpitations. Some pathways may activate a region of ventricular muscle earlier than would normally occur, referred to as pre-excitation, and this may be seen on an electrocardiogram. The combination of an accessory pathway that causes pre-excitation with arrhythmias is known as Wolff–Parkinson–White syndrome.

Left anterior fascicular block (LAFB) is an abnormal condition of the left ventricle of the heart, related to, but distinguished from, left bundle branch block (LBBB).
A left posterior fascicular block (LPFB), also known as left posterior hemiblock (LPH), is a condition where the left posterior fascicle, which travels to the inferior and posterior portion of the left ventricle, does not conduct the electrical impulses from the atrioventricular node. The wave-front instead moves more quickly through the left anterior fascicle and right bundle branch, leading to a right axis deviation seen on the ECG.

An intraventricular block is a heart conduction disorder — heart block of the ventricles of the heart. An example is a right bundle branch block, right fascicular block, bifascicular block, trifascicular block.

Vectorcardiography (VCG) is a method of recording the magnitude and direction of the electrical forces that are generated by the heart by means of a continuous series of vectors that form curving lines around a central point.

In electrocardiography, left axis deviation (LAD) is a condition wherein the mean electrical axis of ventricular contraction of the heart lies in a frontal plane direction between −30° and −90°. This is reflected by a QRS complex positive in lead I and negative in leads aVF and II.