Pathophysiology
Histological findings include granulation tissue, microrupture, degenerative changes, and there is no traditional inflammation. As a consequence, “lateral elbow tendinopathy or tendinosis” is used instead of “lateral epicondylitis”. [7]
Examination of tennis elbow tissue reveals noninflammatory tissue, so the term “angiofibroblastic tendinosis” is used. [8]
Cultures from tendinopathic tendons contain an increased production of type III collagen. [9] [10]
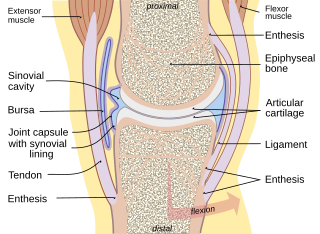
Longitudinal sonogram of the lateral elbow displays thickening and heterogeneity of the common extensor tendon that is consistent with tendinosis, as the ultrasound reveals calcifications, intrasubstance tears, and marked irregularity of the lateral epicondyle. Although the term “epicondylitis” is frequently used to describe this disorder, most histopathologic findings of studies have displayed no evidence of an acute, or a chronic inflammatory process. Histologic studies have demonstrated that this condition is the result of tendon degeneration, which causes normal tissue to be replaced by a disorganized arrangement of collagen. Therefore, the disorder is more appropriately referred to as “tendinosis” or “tendinopathy” rather than “tendinitis.” [11]
Colour Doppler ultrasound reveals structural tendon changes, with vascularity and hypo-echoic areas that correspond to the areas of pain in the extensor origin. [12]
Load-induced non-rupture tendinopathy in humans is associated with an increase in the ratio of collagen III:I proteins, a shift from large to small diameter collagen fibrils, buckling of the collagen fascicles in the tendon extracellular matrix, and buckling of the tenocyte cells and their nuclei. [13]
Diagnosis
Symptoms can vary from an ache or pain and stiffness to the local area of the tendon, or a burning that surrounds the whole joint around the affected tendon. With this condition, the pain is usually worse during and after activity, and the tendon and joint area can become stiffer the following day as swelling impinges on the movement of the tendon. Many patients report stressful situations in their life in correlation with the beginnings of pain, which may contribute to the symptoms.
Swelling in a region of micro damage or partial tear may be detected visually or by touch.
Medical imaging
Ultrasound imaging can be used to evaluate tissue strain, as well as other mechanical properties. [14]
Ultrasound-based techniques are becoming more popular because of its affordability, safety, and speed. Ultrasound can be used for imaging tissues, and the sound waves can also provide information about the mechanical state of the tissue. [15]
Increased water content and disorganized collagen matrix in tendon lesions may be detected by ultrasonography or magnetic resonance imaging.
Research
Eccentric loading and extracorporeal shockwave therapy are currently being researched as possible treatments for tendinosis. One study found the two modalities to be equally effective in treating tendinosis of the Achilles tendon and more effective than a 'wait and see' approach. [21] Other treatments for which research is on-going include vitamin E, vitamin B6, nitric oxide, Platelet Rich Plasma (PRP), [22] and stem cell injections.
Vitamin C
One study found increased Achilles tendon healing in rats supplemented with high doses of vitamin C, which is needed for collagen synthesis. [23]
Vitamin E
Vitamin E has been found to increase the activity of fibroblasts, leading to increased collagen fibrils and synthesis, which seems to speed up the regeneration and increase the regenerative capacity of tendons. [24] [25]
Nitric oxide
Nitric oxide (NO) also appears to play a role in tendon healing [26] and inhibition of its synthesis impairs tendon healing. [27] The use of a nitric oxide delivery system (glyceryl trinitrate patches) applied over the area of maximal tenderness was tested in three clinical trials for the treatment of tendinopathies and was found to significantly reduce pain and increase range of motion and strength. [28]
One study found that arginine supplementation, which may possibly increase NO signaling, [29] was able to increase the speed of tendon healing [30]
Soft tissue mobilization
Augmented Soft Tissue Mobilization (ASTM) is a form of manual therapy that has been shown in studies on rats to speed the healing of tendons by increasing fibroblast activity. [31] [32] One case study showed ASTM resulting in full recovery in the case of an athlete suffering from chronic ankle pain and fibrosis, after an unsuccessful course of surgery and conventional physical therapy. [33]
Eccentric loading
A promising line of therapy involves eccentric loading exercises involving lengthening muscular contractions. [34]
Inflatable brace
The use of an inflatable brace (AirHeel) was shown to be as effective as eccentric loading in the treatment of chronic Achilles tendinopathy. Both modalities produced significant reduction in pain scores, but their combination was no more effective than either treatment alone. [35]
Tendon bioengineering
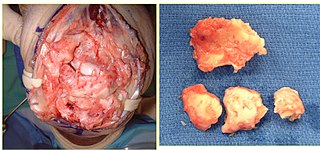
The future of non-surgical care for tendinosis is likely bioengineering. Ligament reconstruction is possible using mesenchymal stem cells and a silk scaffold. [39] These same stem cells were capable of seeding repair of damaged animal tendons. [40] Autologous tenocyte implantation is currently being tested for tendinosis. There is a large randomized, double-blind, placebo controlled trial being conducted in the Netherlands to test the safety and efficacy of tenocyte therapy. Results from the trial are expected by April 2013.
Autologous tenocyte injection
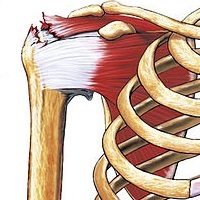
A study investigated autologous tenocyte injection for the treatment of severe, chronic resistant lateral epicondylitis. A needle biopsy was used on the patellar tendon, and the extracted tendon cells were expanded by in vitro culture. The autologous tenocytes were sorted and purified by real-time polymerase chain reaction, and amplified by flow cytometry. The tenocytes were then injected into the injured tendinopathy site, which was the origin of the extensor carpi radialis brevis tendon, under the guidance of an ultrasound. After the autologous tenocyte injection treatment, patients with chronic lateral epicondylitis showed improved clinical function and structural repair at the origin of the common extensor tendon. [41]
Nonbulbar dermal sheath cells
RepliCel has planned a Phase 1/2 Achilles tendinosis clinical trial using fibroblasts that are isolated from the nonbulbar dermal sheath cells of a hair follicle, and is recruiting in Q1 2015. The tendon treatment will be tested in approximately 28 subjects. Nonbulbar dermal sheath cells are used because they produce more type I collagen than fibroblasts that are derived from adipose tissue. Type I collagen is the primary collagen in tendons. Nonbulbar dermal sheath cells will be replicated, and then reintroduced into the wounded tendons with ultrasound. After the injections, subjects will be assessed for pain, safety, and function, as well as changes in interstitial tears, tendon thickness, echotexture, and neovascularity. [42] [43]
Injections of microRNA
Scientists found that mir-29a, a single microRNA, through its interaction with a protein, interleukin 33, plays a key role in regulating the production of collagens in tendon disease. Loss of miR29a from human tendons results in an increase in collagen type-3 production, which is a key feature of tendon disease. The replacement of miR-29a in the damaged tendon cells in the laboratory restores collagen production to pre injury levels. A trial will put injections of microRNA – small molecules that help regulate gene expression – into the tendon to decrease the production of type 3 collagen and switch to type-1. [44]
Allogenic adipose-derived mesenchymal stem cells
As of November 2013, researchers at the Seoul National University Hospital will be looking to recruit participants into a clinical trial to evaluate the efficacy of allogenic adipose-derived mesenchymal stem cells (ALLO-ASC) for the treatment of a lateral epicondylitis tendon injury where the duration of the symptoms is over six months. Adipose-derived mesenchymal stem cells will be administrated to the patients with lateral epicondylitis (tennis elbow) by an ultrasonographic-guided injection. [45]
Elastography ultrasound
Researchers have tried to analyze tissue strain and mechanical properties using elastography, which is an acoustical imaging technique that measures strain distributions in tissues that result from stress or compression of the tissue. Strain is inversely related to stiffness, so under a given amount of stress, tissue that displays less strain is assumed to be stiffer than tissue that exhibits more strain. Elastography is therefore an indirect method to estimate tissue stiffness. [14]
One limitation of elastography is that it is inherently linear when ultrasound wave velocity and the material properties do not change during the strain measurement. This is a problem in soft tissues like tendons, as they are nonlinear in stiffness, and can undergo large deformations in activity. Elastography measures strain, and to more completely described the mechanical behavior, more data, like stiffness or stress would be required. [14]
Acoustoelastography ultrasound
Acoustoelastic theory is based on the principle that the acoustic properties of a material are altered as the material is loaded and deformed. The properties can be measured as a change in amplitude and wave velocity. [15]
With the use of A-mode ultrasound, researchers have derived an acoustic relationship between reflected wave amplitude, and strain-dependent stiffness and stress in a deformed material. [15]
As tendon tension increases, the intensity of reflected ultrasonic echoes increases. The increased intensity results in a brighter B-mode ultrasound image. [14]
Acoustoelastography is an ultrasound technique that relates ultrasonic wave amplitude changes to the mechanical properties of a tendon. [46]
It is an ultrasound-based model that can be used evaluate tendon function. Gradual deformations of a tendon can produce cine loops, where changes in echo intensity can be observed. By analyzing the echo intensity changes with Acoustoelastography, one can deduce the stiffness gradient, which is the rate of change of normalised stiffness as a function of strain. [47]
EchoSoft ultrasound software from the Wisconsin Alumni Research Foundation and Echometrix applies the theory of acoustoelasticity to measure musculoskeletal (tendon and ligament) tissue. The software examines previously unused information found by ultrasound waves to quantify the extent of musculoskeletal injuries, or a patient's progress in a healing process. [48]
Ultrasonic Percutaneous Tenotomy
Percutaneous ultrasonic tenotomy provided continued pain relief and functional improvement for recalcitrant tennis elbow at a 3-year follow-up. [49]
Other animals
Bowed tendon is a horseman's term for tendinitis (inflammation) and tendinosis (degeneration), most commonly seen in the superficial digital flexor tendon in the front leg of horses.
Diagnosis
When the superficial digital flexor tendon of horses is damaged, there is a thickening of the tendon, giving it a bowed appearance when the leg is viewed from the side.
Medical imaging
A study tested the repeatability and feasibility of using acoustoelastography for in vivo measurement of stiffness gradients in the superficial digital flexor tendons (SDFTs) of clinically normal horses. The results show that acoustoelastography is a repeatable and feasible technique for measuring stiffness gradients of superficial digital flexor tendons in clinically normal horses, and acoustoelastography has the potential to be used for comparing diseased and healthy tendon states. [50]
A report describes the use of acoustoelastography to monitor the mechanical healing of an Achilles tendon laceration in a dog after suture repair. Serial acoustoelastography examinations of the tendon showed that mechanical properties improved throughout the recovery period. At 29 weeks, the mechanical properties of the repaired tendon were similar to that of the normal contralateral Achilles mechanism. [46]
A study shows that acoustoelastography is a repeatable and feasible method for measuring stiffness gradients in equine superficial digital flexor tendons. [47]
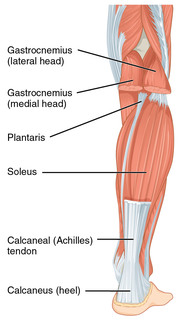
The acoustoelastic strain gauge is an ultrasound-based tissue evaluation technique that relates echo intensity changes that are observed during the stretching or relaxation tendons to the mechanical properties of the tissue. The method deduces stiffness gradient (the rate of change of normalized stiffness as a function of tissue strain) by evaluating the ultrasound dynamic images that are captured from tissue as it gradually deforms. Acoustoelastic strain gauge has been shown to accurately model stiffness and strain within tendons in vitro. To determine the repeatability and feasibility of in vivo ASG measurements of canine tendon function, stiffness gradients for the gastrocnemius tendons of dogs were recorded. Findings indicate that acoustoelastic strain gauge is a repeatable and feasible technique for measuring stiffness gradients in canine tendons. [51]
Pathophysiology
Achilles tendons in rats were studied with acoustoelastography ultrasound. After a tendon injury, and during tendon healing, vascularity changes and cellular activity are vital to the formation of granular tissue in the tendon gap, and the subsequent development of neo-tendinous tissue that replaces damaged native tissue. Normal, intact tendon is composed mainly of type I collagen, and type III collagen increases after injury. Another study has recorded an association between collagen fibers and echogenicity tendon during Achilles tendon healing. [52]
This report further indicates that a decrease in type I procollagen (and increase in type III collagen and periostin) correlates to reduced strength, echo intensity, and normalized stiffness. It shows that tissue normalized stiffness is linearly correlated to procollagen I, while echo intensity is seen to be nonlinearly correlated to type I procollagen. Furthermore, the increase in M1 macrophages, blood vessels, and proliferating cells that occur within two weeks of the injury are associated with a formation of granulation tissue. Ultimate stress, echo intensity, and normalized stiffness are all their lowest during these times. The results assert that the reduction in stress and normalized stiffness that is measured by ultrasonic and mechanical methods correlate well with the biological aspect of tendon healing. [52]
Treatment
Mesenchymal stem cells, derived from a horse's bone marrow or fat, are currently being used for tendon repair in horses. [53]