Arthritis is a term often used to mean any disorder that affects joints. Symptoms generally include joint pain and stiffness. Other symptoms may include redness, warmth, swelling, and decreased range of motion of the affected joints. In some types of arthritis, other organs are also affected. Onset can be gradual or sudden.

Rheumatoid arthritis (RA) is a long-term autoimmune disorder that primarily affects joints. It typically results in warm, swollen, and painful joints. Pain and stiffness often worsen following rest. Most commonly, the wrist and hands are involved, with the same joints typically involved on both sides of the body. The disease may also affect other parts of the body, including skin, eyes, lungs, heart, nerves, and blood. This may result in a low red blood cell count, inflammation around the lungs, and inflammation around the heart. Fever and low energy may also be present. Often, symptoms come on gradually over weeks to months.

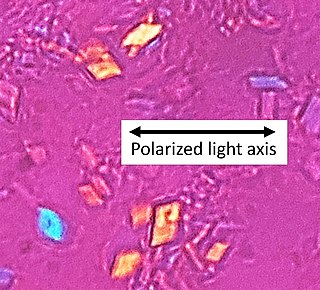
Gout is a form of inflammatory arthritis characterized by recurrent attacks of a red, tender, hot and swollen joint, caused by the deposition of needle-like crystals of uric acid known as monosodium urate crystals. Pain typically comes on rapidly, reaching maximal intensity in less than 12 hours. The joint at the base of the big toe is affected (Podagra) in about half of cases. It may also result in tophi, kidney stones, or kidney damage.
Rheumatology is a branch of medicine devoted to the diagnosis and management of disorders whose common feature is inflammation in the bones, muscles, joints, and internal organs. Rheumatology covers more than 100 different complex diseases, collectively known as rheumatic diseases, which includes many forms of arthritis as well as lupus and Sjögren's syndrome. Doctors who have undergone formal training in rheumatology are called rheumatologists.

Tietze syndrome is a benign inflammation of one or more of the costal cartilages. It was first described in 1921 by German surgeon Alexander Tietze and was subsequently named after him. The condition is characterized by tenderness and painful swelling of the anterior (front) chest wall at the costochondral, sternocostal, or sternoclavicular junctions. Tietze syndrome affects the true ribs and has a predilection for the 2nd and 3rd ribs, commonly affecting only a single joint.
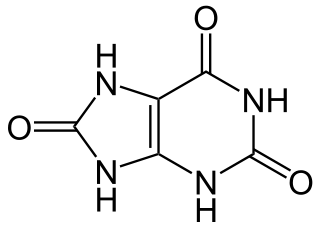
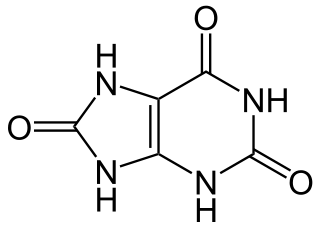
Hyperuricaemia or hyperuricemia is an abnormally high level of uric acid in the blood. In the pH conditions of body fluid, uric acid exists largely as urate, the ion form. Serum uric acid concentrations greater than 6 mg/dL for females, 7 mg/dL for men, and 5.5 mg/dL for youth are defined as hyperuricemia. The amount of urate in the body depends on the balance between the amount of purines eaten in food, the amount of urate synthesised within the body, and the amount of urate that is excreted in urine or through the gastrointestinal tract. Hyperuricemia may be the result of increased production of uric acid, decreased excretion of uric acid, or both increased production and reduced excretion.
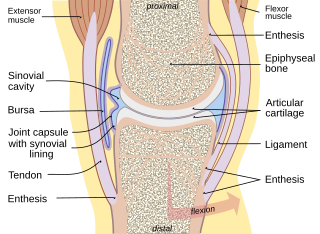
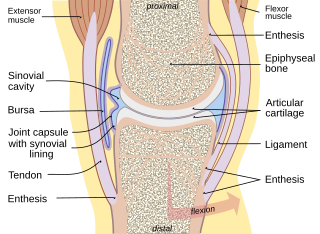
Synovial fluid, also called synovia,[help 1] is a viscous, non-Newtonian fluid found in the cavities of synovial joints. With its egg white–like consistency, the principal role of synovial fluid is to reduce friction between the articular cartilage of synovial joints during movement. Synovial fluid is a small component of the transcellular fluid component of extracellular fluid.

A tophus is a deposit of monosodium urate crystals, in people with longstanding high levels of uric acid (urate) in the blood, a condition known as hyperuricemia. Tophi are pathognomonic for the disease gout. Most people with tophi have had previous attacks of acute arthritis, eventually leading to the formation of tophi. Chronic tophaceous gout is known as Harrison Syndrome.
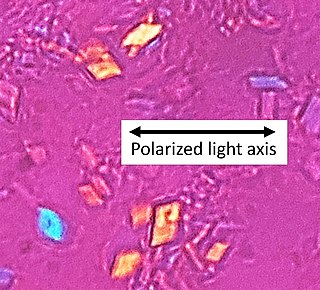
Calcium pyrophosphate dihydrate (CPPD) crystal deposition disease, also known as pseudogout and pyrophosphate arthropathy, is a rheumatologic disease which is thought to be secondary to abnormal accumulation of calcium pyrophosphate dihydrate crystals within joint soft tissues. The knee joint is most commonly affected. The disease is metabolic in origin and its treatment remains symptomatic.

An arthropathy is a disease of a joint.

Relapsing polychondritis is a systemic disease characterized by repeated episodes of inflammation and in some cases deterioration of cartilage. The disease can be life-threatening if the respiratory tract, heart valves, or blood vessels are affected. The exact mechanism is poorly understood.

Reactive arthritis, also known as Reiter's syndrome, is a form of inflammatory arthritis that develops in response to an infection in another part of the body (cross-reactivity). Coming into contact with bacteria and developing an infection can trigger the disease. By the time the patient presents with symptoms, often the "trigger" infection has been cured or is in remission in chronic cases, thus making determination of the initial cause difficult.
Mixed connective tissue disease, commonly abbreviated as MCTD, is an autoimmune disease characterized by the presence of elevated blood levels of a specific autoantibody, now called anti-U1 ribonucleoprotein (RNP) together with a mix of symptoms of systemic lupus erythematosus (SLE), scleroderma, and polymyositis. The idea behind the "mixed" disease is that this specific autoantibody is also present in other autoimmune diseases such as systemic lupus erythematosus, polymyositis, scleroderma, etc. MCTD was characterized as an individual disease in 1972 by Sharp et al., and the term was introduced by Leroy in 1980.
Palindromic rheumatism (PR) is a syndrome characterised by recurrent, self-resolving inflammatory attacks in and around the joints, and consists of arthritis or periarticular soft tissue inflammation. The course is often acute onset, with sudden and rapidly developing attacks or flares. There is pain, redness, swelling, and disability of one or multiple joints. The interval between recurrent palindromic attacks and the length of an attack is extremely variable from few hours to days. Attacks may become more frequent with time but there is no joint damage after attacks. It is thought to be an autoimmune disease, possibly an abortive form of rheumatoid arthritis.

Anti-citrullinated protein antibodies (ACPAs) are autoantibodies that are directed against peptides and proteins that are citrullinated. They are present in the majority of patients with rheumatoid arthritis. Clinically, cyclic citrullinated peptides (CCP) are frequently used to detect these antibodies in patient serum or plasma.

Sir Alfred Baring Garrod was an English physician.

Knee pain is pain in or around the knee.

Jaccoud arthropathy (JA), is a chronic non-erosive reversible joint disorder that may occur after repeated bouts of arthritis. It is caused by inflammation of the joint capsule and subsequent fibrotic retraction, causing ulnar deviation of the fingers, through metacarpophalangeal joint (MCP) subluxation, primarily of the ring and little-finger. Joints in the feet, knees and shoulders may also get affected. It is commonly associated with systemic lupus erythematosus (SLE), and occurs in roughly 5% of all cases.

An antiarthritic is any drug used to relieve or prevent arthritic symptoms, such as joint pain or joint stiffness. Depending on the antiarthritic drug class, it is used for managing pain, reducing inflammation or acting as an immunosuppressant. These drugs are typically given orally, topically or through administration by injection. The choice of antiarthritic medication is often determined by the nature of arthritis, the severity of symptoms as well as other factors, such as the tolerability of side effects.

Trabecular edema, also known as bone marrow edema (BME), is a traditional term describing the interstitial fluid accumulation at the trabecular bone marrow. The term was first used in 1988, referring to the changes in the bone marrow due to inflammation. Bone marrow edema was later renamed to bone marrow lesion (BML), as later studies show that the increased fluid content in the trabecular bone was more likely caused by inflammatory responses instead of fluid influx. Hence, this narrows down the condition to the damage at the articular surface of the trabecular bones. Despite so, the terms BME and BML are still used interchangeably in radiology.