Arthritis is a term often used to mean any disorder that affects joints. Symptoms generally include joint pain and stiffness. Other symptoms may include redness, warmth, swelling, and decreased range of motion of the affected joints. In some types of arthritis, other organs are also affected. Onset can be gradual or sudden.

Rheumatoid arthritis (RA) is a long-term autoimmune disorder that primarily affects joints. It typically results in warm, swollen, and painful joints. Pain and stiffness often worsen following rest. Most commonly, the wrist and hands are involved, with the same joints typically involved on both sides of the body. The disease may also affect other parts of the body. This may result in a low red blood cell count, inflammation around the lungs, and inflammation around the heart. Fever and low energy may also be present. Often, symptoms come on gradually over weeks to months.
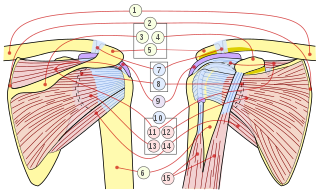
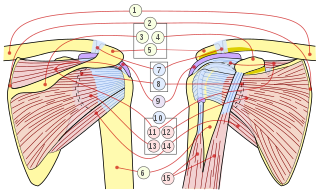
In anatomy, the rotator cuff is a group of muscles and their tendons that act to stabilize the shoulder and allow for its extensive range of motion. Of the seven scapulohumeral muscles, four make up the rotator cuff. The four muscles are the supraspinatus muscle, the infraspinatus muscle, teres minor muscle, and the subscapularis muscle.

Tendinopathy, also known as tendinitis or tendonitis, is a type of tendon disorder that results in pain, swelling, and impaired function. The pain is typically worse with movement. It most commonly occurs around the shoulder, elbow, wrist, hip, knee, or ankle.

Trigger finger, also known as stenosing tenosynovitis, is a disorder characterized by catching or locking of the involved finger. Pain may occur in the palm of the hand or knuckles. The name is due to the popping sound made by the affected finger when moved. Most commonly the ring finger or thumb is affected.

Shoulder problems including pain, are one of the more common reasons for physician visits for musculoskeletal symptoms. The shoulder is the most movable joint in the body. However, it is an unstable joint because of the range of motion allowed. This instability increases the likelihood of joint injury, often leading to a degenerative process in which tissues break down and no longer function well.

Osteoarthritis (OA) is a type of joint disease that results from breakdown of joint cartilage and underlying bone. The most common symptoms are joint pain and stiffness. Usually the symptoms progress slowly over years. Initially they may only occur after exercise, but can become constant over time. Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs; the knee and hip joints; and the joints of the neck and lower back. Joints on one side of the body are often more affected than those on the other. The symptoms can interfere with work and normal daily activities. Unlike some other types of arthritis, only the joints, not internal organs, are affected.
Diabetic neuropathy refers to various types of nerve damage associated with diabetes mellitus. Symptoms depend on the site of nerve damage and can include motor changes such as weakness; sensory symptoms such as numbness, tingling, or pain; or autonomic changes such as urinary symptoms. These changes are thought to result from microvascular injury involving small blood vessels that supply nerves. Relatively common conditions which may be associated with diabetic neuropathy include distal symmetric polyneuropathy; third, fourth, or sixth cranial nerve palsy; mononeuropathy; mononeuropathy multiplex; diabetic amyotrophy; and autonomic neuropathy.

Tennis elbow, also known as lateral epicondylitis, is a condition in which the outer part of the elbow becomes painful and tender. The pain may also extend into the back of the forearm and grip strength may be weak. Onset of symptoms is generally gradual. Golfer's elbow is a similar condition that affects the inside of the elbow.

Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related wear and tear of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.
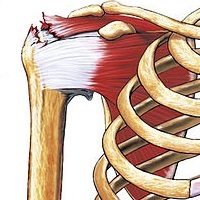
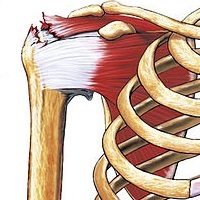
A rotator cuff tear is an injury of one or more of the tendons or muscles of the rotator cuff of the shoulder. Symptoms may include shoulder pain, which is often worse with movement, or weakness. This may limit people’s ability to brush their hair or put on clothing. Clicking may also occur with movement of the arm.

Electrotherapy is the use of electrical energy as a medical treatment. In medicine, the term electrotherapy can apply to a variety of treatments, including the use of electrical devices such as deep brain stimulators for neurological disease. The term has also been applied specifically to the use of electric current to speed wound healing. Additionally, the term "electrotherapy" or "electromagnetic therapy" has also been applied to a range of alternative medical devices and treatments.
Myofascial pain syndrome (MPS), also known as chronic myofascial pain (CMP), is a syndrome characterized by chronic pain in multiple myofascial trigger points ("knots") and fascial constrictions. It can appear in any body part. Symptoms of a myofascial trigger points include: focal point tenderness, reproduction of pain upon trigger point palpation, hardening of the muscle upon trigger point palpation, pseudo-weakness of the involved muscle, referred pain, and limited range of motion following approximately 5 seconds of sustained trigger point pressure.
Greater trochanteric pain syndrome (GTPS), is inflammation of the trochanteric bursa, a part of the hip.

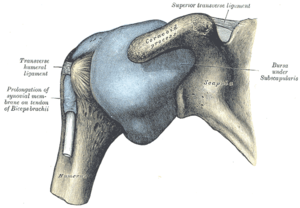
Subacromial bursitis is a condition caused by inflammation of the bursa that separates the superior surface of the supraspinatus tendon from the overlying coraco-acromial ligament, acromion, and coracoid and from the deep surface of the deltoid muscle. The subacromial bursa helps the motion of the supraspinatus tendon of the rotator cuff in activities such as overhead work.

Calcific tendinitis is a form of tendinitis, a disorder characterized by deposits of hydroxyapatite in any tendon of the body, but most commonly in the tendons of the rotator cuff (shoulder), causing pain and inflammation. The condition is related to and may cause adhesive capsulitis.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. This can result in pain, weakness, numbness, or difficulty controlling specific muscles.
Arthrofibrosis has been described in most joints like knee, hip, ankle, foot joints, shoulder, elbow, wrist, hand joints as well as spinal vertebrae. In the knee, it can happen after knee injury or surgery. There is excessive scar tissue formation within the joint and surrounding soft tissues leading to painful restriction of joint motion that persists despite physical therapy and rehabilitation. The scar tissue can involve only a part of the knee joint or the whole knee. The scar tissue may be located inside the knee joint or may involve the soft tissue structures around the knee joint. Arthrofibrosis may arise without an obvious cause or it may follow a known cause.

The capsule of the glenohumeral (shoulder) joint is the articular capsule of the shoulder. It completely surrounds the joint. It is attached above to the circumference of the glenoid cavity beyond the glenoidal labrum, and below to the anatomical neck of the humerus, approaching nearer to the articular cartilage above than in the rest of its extent.

Shoulder impingement syndrome is a syndrome involving tendonitis of the rotator cuff muscles as they pass through the subacromial space, the passage beneath the acromion. It is particularly associated with tendonitis of the supraspinatus muscle. This can result in pain, weakness, and loss of movement at the shoulder.