Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), myocardial ischemia, or simply heart disease, involves the reduction of blood flow to the heart muscle due to build-up of atherosclerotic plaque in the arteries of the heart. It is the most common of the cardiovascular diseases. Types include stable angina, unstable angina, and myocardial infarction.
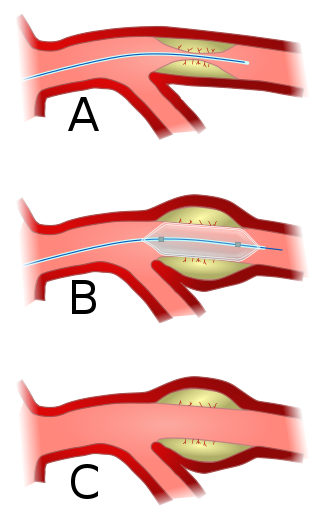
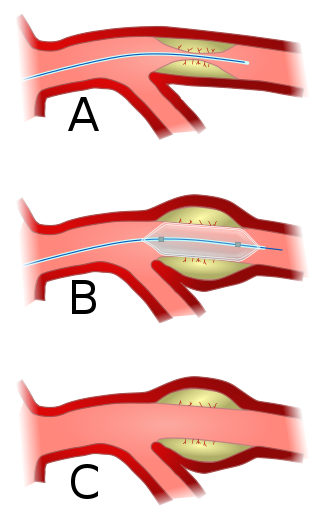
Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis.

Electrocardiography is the process of producing an electrocardiogram, a recording of the heart's electrical activity through repeated cardiac cycles. It is an electrogram of the heart which is a graph of voltage versus time of the electrical activity of the heart using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including:

Coronary artery bypass surgery, also known as coronary artery bypass graft, is a surgical procedure to treat coronary artery disease (CAD), the buildup of plaques in the arteries of the heart. It can relieve chest pain caused by CAD, slow the progression of CAD, and increase life expectancy. It aims to bypass narrowings in heart arteries by using arteries or veins harvested from other parts of the body, thus restoring adequate blood supply to the previously ischemic heart.

In electrocardiography, the T wave represents the repolarization of the ventricles. The interval from the beginning of the QRS complex to the apex of the T wave is referred to as the absolute refractory period. The last half of the T wave is referred to as the relative refractory period or vulnerable period. The T wave contains more information than the QT interval. The T wave can be described by its symmetry, skewness, slope of ascending and descending limbs, amplitude and subintervals like the Tpeak–Tend interval.

The QRS complex is the combination of three of the graphical deflections seen on a typical electrocardiogram. It is usually the central and most visually obvious part of the tracing. It corresponds to the depolarization of the right and left ventricles of the heart and contraction of the large ventricular muscles.

Acute coronary syndrome (ACS) is a syndrome due to decreased blood flow in the coronary arteries such that part of the heart muscle is unable to function properly or dies. The most common symptom is centrally located pressure-like chest pain, often radiating to the left shoulder or angle of the jaw, and associated with nausea and sweating. Many people with acute coronary syndromes present with symptoms other than chest pain, particularly women, older people, and people with diabetes mellitus.

Variant angina, also known as Prinzmetal angina,vasospastic angina, angina inversa, coronary vessel spasm, or coronary artery vasospasm, is a syndrome typically consisting of angina. Variant angina differs from stable angina in that it commonly occurs in individuals who are at rest or even asleep, whereas stable angina is generally triggered by exertion or intense exercise. Variant angina is caused by vasospasm, a narrowing of the coronary arteries due to contraction of the heart's smooth muscle tissue in the vessel walls. In comparison, stable angina is caused by the permanent occlusion of these vessels by atherosclerosis, which is the buildup of fatty plaque and hardening of the arteries.

Percutaneous coronary intervention (PCI) is a minimally invasive non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The procedure is used to place and deploy coronary stents, a permanent wire-meshed tube, to open narrowed coronary arteries. PCI is considered 'non-surgical' as it uses a small hole in a peripheral artery (leg/arm) to gain access to the arterial system, an equivalent surgical procedure would involve the opening of the chest wall to gain access to the heart area. The term 'coronary angioplasty with stent' is synonymous with PCI. The procedure visualises the blood vessels via fluoroscopic imaging and contrast dyes. PCI is performed by an interventional cardiologists in a catheterization laboratory setting.

A drug-eluting stent (DES) is a thin tube that is used to treat narrowed arteries in medical procedures. It releases drugs to prevent the growth of scar tissue and reduce the risk of stent restenosis, which is the narrowing of the stented area of an artery after treatment. A drug-eluting stent is different from other types of stents because it has a coating that delivers medication directly to the arterial wall. A DES is often made of metal alloys and can be inserted into blocked or narrowed arteries through a catheter placed in a peripheral artery, such as in the arm or leg. DES is fully integrated with a catheter delivery system and is viewed as one integrated medical device.
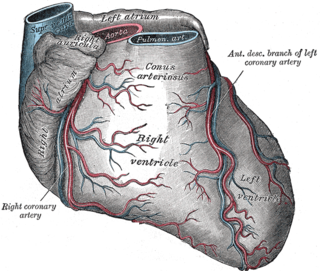
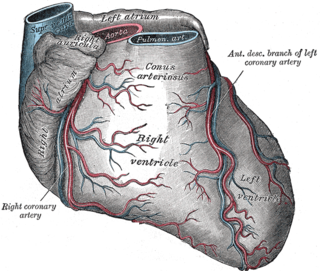
The left anterior descending artery is a branch of the left coronary artery. It supplies the anterior portion of the left ventricle. It provides about half of the arterial supply to the left ventricle and is thus considered the most important vessel supplying the left ventricle. Blockage of this artery is often called the widow-maker infarction due to a high risk of death.
Door-to-balloon is a time measurement in emergency cardiac care (ECC), specifically in the treatment of ST segment elevation myocardial infarction. The interval starts with the patient's arrival in the emergency department, and ends when a catheter guidewire crosses the culprit lesion in the cardiac cath lab. Because of the adage that "time is muscle", meaning that delays in treating a myocardial infarction increase the likelihood and amount of cardiac muscle damage due to localised hypoxia, ACC/AHA guidelines recommend a door-to-balloon interval of no more than 90 minutes. As of 2006 in the United States, fewer than half of STEMI patients received reperfusion with primary percutaneous coronary intervention (PCI) within the guideline-recommended timeframe. It has become a core quality measure for the Joint Commission on Accreditation of Healthcare Organizations (TJC).

Wellens' syndrome is an electrocardiographic manifestation of critical proximal left anterior descending (LAD) coronary artery stenosis in people with unstable angina. Originally thought of as two separate types, A and B, it is now considered an evolving wave form, initially of biphasic T wave inversions and later becoming symmetrical, often deep, T wave inversions in the anterior precordial leads.

A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops in one of the coronary arteries of the heart, causing infarction to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often such pain occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat, feeling tired, and decreased level of consciousness. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest.

ST elevation refers to a finding on an electrocardiogram wherein the trace in the ST segment is abnormally high above the baseline.

Spontaneous coronary artery dissection (SCAD) is an uncommon but potentially lethal condition in which one of the coronary arteries that supply the heart, spontaneously develops a blood collection, or hematoma, within the artery wall due to a tear in the wall. SCAD is one of the arterial dissections that can occur.

Reperfusion therapy is a medical treatment to restore blood flow, either through or around, blocked arteries, typically after a heart attack. Reperfusion therapy includes drugs and surgery. The drugs are thrombolytics and fibrinolytics used in a process called thrombolysis. Surgeries performed may be minimally-invasive endovascular procedures such as a percutaneous coronary intervention (PCI), which involves coronary angioplasty. The angioplasty uses the insertion of a balloon and/or stents to open up the artery. Other surgeries performed are the more invasive bypass surgeries that graft arteries around blockages.

Electrocardiography in suspected myocardial infarction has the main purpose of detecting ischemia or acute coronary injury in emergency department populations coming for symptoms of myocardial infarction (MI). Also, it can distinguish clinically different types of myocardial infarction.
A diagnosis of myocardial infarction is created by integrating the history of the presenting illness and physical examination with electrocardiogram findings and cardiac markers. A coronary angiogram allows visualization of narrowings or obstructions on the heart vessels, and therapeutic measures can follow immediately. At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.

Management of acute coronary syndrome is targeted against the effects of reduced blood flow to the affected area of the heart muscle, usually because of a blood clot in one of the coronary arteries, the vessels that supply oxygenated blood to the myocardium. This is achieved with urgent hospitalization and medical therapy, including drugs that relieve chest pain and reduce the size of the infarct, and drugs that inhibit clot formation; for a subset of patients invasive measures are also employed. Basic principles of management are the same for all types of acute coronary syndrome. However, some important aspects of treatment depend on the presence or absence of elevation of the ST segment on the electrocardiogram, which classifies cases upon presentation to either ST segment elevation myocardial infarction (STEMI) or non-ST elevation acute coronary syndrome (NST-ACS); the latter includes unstable angina and non-ST elevation myocardial infarction (NSTEMI). Treatment is generally more aggressive for STEMI patients, and reperfusion therapy is more often reserved for them. Long-term therapy is necessary for prevention of recurrent events and complications.