Arthritis is a term often used to mean any disorder that affects joints. Symptoms generally include joint pain and stiffness. Other symptoms may include redness, warmth, swelling, and decreased range of motion of the affected joints. In some types of arthritis, other organs are also affected. Onset can be gradual or sudden.

In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

Tenosynovitis is the inflammation of the fluid-filled sheath that surrounds a tendon, typically leading to joint pain, swelling, and stiffness. Tenosynovitis can be either infectious or noninfectious. Common clinical manifestations of noninfectious tenosynovitis include de Quervain tendinopathy and stenosing tenosynovitis

Bursitis is the inflammation of one or more bursae of synovial fluid in the body. They are lined with a synovial membrane that secretes a lubricating synovial fluid. There are more than 150 bursae in the human body. The bursae rest at the points where internal functionaries, such as muscles and tendons, slide across bone. Healthy bursae create a smooth, almost frictionless functional gliding surface making normal movement painless. When bursitis occurs, however, movement relying on the inflamed bursa becomes difficult and painful. Moreover, movement of tendons and muscles over the inflamed bursa aggravates its inflammation, perpetuating the problem. Muscle can also be stiffened.

A malignant peripheral nerve sheath tumor (MPNST) is a form of cancer of the connective tissue surrounding nerves. Given its origin and behavior it is classified as a sarcoma. About half the cases are diagnosed in people with neurofibromatosis; the lifetime risk for an MPNST in patients with neurofibromatosis type 1 is 8–13%. MPNST with rhabdomyoblastomatous component are called malignant triton tumors.

Synovial osteochondromatosis (SOC) is a rare disease that creates a benign change or proliferation in the synovium or joint-lining tissue, which changes to form bone-forming cartilage. In most occurrences, there is only one joint affected, either the knee, the hip, or the elbow. Rarely involves the TMJ.

Osteochondromas are the most common benign tumors of the bones. The tumors take the form of cartilage-capped bony projections or outgrowth on the surface of bones exostoses. It is characterized as a type of overgrowth that can occur in any bone where cartilage forms bone. Tumors most commonly affect long bones about the knee and in the forearm. Additionally, flat bones such as the pelvis and scapula may be affected. Hereditary multiple exostoses usually present during childhood. Yet, the vast majority of affected individuals become clinically manifest by the time they reach adolescence. Osteochondromas occur in 3% of the general population and represent 35% of all benign tumors and 8% of all bone tumors. The majority of these tumors are solitary non-hereditary lesions and approximately 15% of osteochondromas occur as hereditary multiple exostoses preferably known as hereditary multiple osteochondromas (HMOs). Osteochondromas do not result from injury and the exact cause remains unknown. Recent research has indicated that multiple osteochondromas is an autosomal dominant inherited disease. Germ line mutations in EXT1 and EXT2 genes located on chromosomes 8 and 11 have been associated with the cause of the disease. The treatment choice for osteochondroma is surgical removal of solitary lesion or partial excision of the outgrowth, when symptoms cause motion limitations or nerve and blood vessel impingements. In hereditary multiple exostoses the indications of surgery are based upon multiple factors that are taken collectively, namely: patient's age, tumor location and number, accompanying symptomatology, esthetic concerns, family history and underlying gene mutation. A variety of surgical procedures have been employed to remedy hereditary multiple exostoses such as osteochondroma excision, bone lengthening, corrective osteotomy and hemiepiphysiodesis. Sometimes a combination of the previous procedures is used. The indicators of surgical success in regard to disease and patient characteristics are greatly disputable. Because most studies of hereditary multiple exostoses are retrospective and of limited sample size with missing data, the best evidence for each of the currently practiced surgical procedures is lacking.

Tarsal tunnel syndrome (TTS), is a compression neuropathy and painful foot condition in which the tibial nerve is compressed as it travels through the tarsal tunnel. This tunnel is found along the inner leg behind the medial malleolus. The posterior tibial artery, tibial nerve, and tendons of the tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles travel in a bundle through the tarsal tunnel. Inside the tunnel, the nerve splits into three segments. One nerve (calcaneal) continues to the heel, the other two continue on to the bottom of the foot. The tarsal tunnel is delineated by bone on the inside and the flexor retinaculum on the outside.
Synovitis is the medical term for inflammation of the synovial membrane. This membrane lines joints that possess cavities, known as synovial joints. The condition is usually painful, particularly when the joint is moved. The joint usually swells due to synovial fluid collection.
This is a shortened version of the thirteenth chapter of the ICD-10: Diseases of the musculoskeletal system and connective tissue. It covers ICD codes M00.0 to M99. All versions of the ICD-10, including the most recent one (2019), can be browsed freely on the website of the World Health Organisation (WHO). The ICD-10 can also be downloaded in PDF-form.
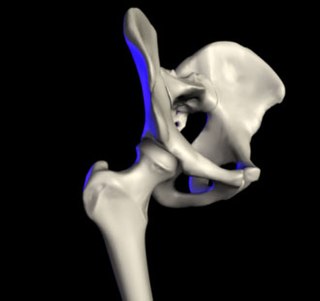
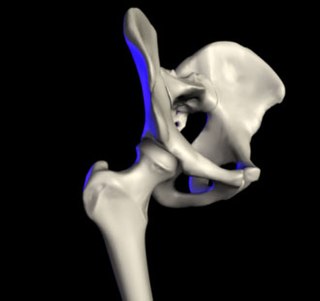
Transient synovitis of hip is a self-limiting condition in which there is an inflammation of the inner lining of the capsule of the hip joint. The term irritable hip refers to the syndrome of acute hip pain, joint stiffness, limp or non-weightbearing, indicative of an underlying condition such as transient synovitis or orthopedic infections. In everyday clinical practice however, irritable hip is commonly used as a synonym for transient synovitis. It should not be confused with sciatica, a condition describing hip and lower back pain much more common to adults than transient synovitis but with similar signs and symptoms.
Synovectomy is a procedure where the synovial tissue surrounding a joint is removed. This procedure is typically recommended to provide relief from a condition in which the synovial membrane or the joint lining becomes inflamed and irritated and is not controlled by medication alone. If arthritis is not controlled, it can lead to irreversible joint damage. The synovial membrane or "synovium" encloses each joint and also secretes a lubricating fluid that allows different joint motions such as rolling, folding and stretching. When the synovium becomes inflamed or irritated, it increases fluid production, resulting in warmth, tenderness, and swelling in and around the joint.
Villonodular synovitis is a type of synovial swelling.
Metallosis is the putative medical condition involving deposition and build-up of metal debris in the soft tissues of the body.
Giant-cell tumor (GCT) of the pelvis is uncommon, accounting for only 1.5 to 6% of cases of GCT. In pelvis ilium is the most common site of involvement; ischium and pubis are less frequently involved. It typically presents in adults between age of 20 to 50 with localized swelling and pain. Females are slightly more affected than males.
Orthopedic surgery is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal injuries, sports injuries, degenerative diseases, infections, bone tumours, and congenital limb deformities. Trauma surgery and traumatology is a sub-specialty dealing with the operative management of fractures, major trauma and the multiply-injured patient.
Cancer pain can be caused by pressure on, or chemical stimulation of, specialised pain-signalling nerve endings called nociceptors, or by damage or illness affecting nerve fibers themselves.

Pain in the hip is the experience of pain in the muscles or joints in the hip/ pelvic region, a condition commonly arising from any of a number of factors. Sometimes it is closely associated with lower back pain.

Intermittent hydrarthrosis (IH), also known as periodic synoviosis, periodic benign synovitis, or periodic hydrarthritis, is a chronic condition of unknown cause characterized by recurring, temporary episodes of fluid accumulation (effusion) in the knee. While the knee is mainly involved, occasionally other joints such as the elbow or ankle can additionally be affected. Fluid accumulation in the joint can be extensive causing discomfort and impairing movement, although affected joints are not usually very painful. While the condition is chronic, it does not appear to progress to more destructive damage of the joint. It seems to affect slightly more women than men.