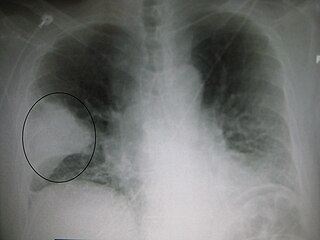
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity of the condition is variable.

Sjögren syndrome or Sjögren's syndrome is a long-term autoimmune disease that affects the body's moisture-producing glands, and often seriously affects other organ systems, such as the lungs, kidneys, and nervous system. Primary symptoms are dryness, pain and fatigue. Other symptoms can include dry skin, vaginal dryness, a chronic cough, numbness in the arms and legs, feeling tired, muscle and joint pains, and thyroid problems. Those affected are also at an increased risk (15%) of lymphoma.
Shortness of breath (SOB), also medically known as dyspnea (AmE) or dyspnoea (BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity", and recommends evaluating dyspnea by assessing the intensity of its distinct sensations, the degree of distress and discomfort involved, and its burden or impact on the patient's activities of daily living. Distinct sensations include effort/work to breathe, chest tightness or pain, and "air hunger". The tripod position is often assumed to be a sign.

Dysautonomia or autonomic dysfunction is a condition in which the autonomic nervous system (ANS) does not work properly. This may affect the functioning of the heart, bladder, intestines, sweat glands, pupils, and blood vessels. Dysautonomia has many causes, not all of which may be classified as neuropathic. A number of conditions can feature dysautonomia, such as Parkinson's disease, multiple system atrophy, dementia with Lewy bodies, Ehlers-Danlos syndromes, autoimmune autonomic ganglionopathy and autonomic neuropathy, HIV/AIDS, autonomic failure, and postural orthostatic tachycardia syndrome.

Cryptococcosis is a potentially fatal fungal infection of mainly the lungs, presenting as a pneumonia, and brain, where it appears as a meningitis. Cough, difficulty breathing, chest pain and fever are seen when the lungs are infected. When the brain is infected, symptoms include headache, fever, neck pain, nausea and vomiting, light sensitivity and confusion or changes in behaviour. It can also affect other parts of the body including skin, where it may appear as several fluid-filled nodules with dead tissue.

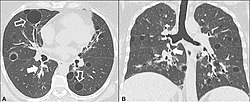
Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

Pulmonary fibrosis is a condition in which the lungs become scarred over time. Symptoms include shortness of breath, a dry cough, feeling tired, weight loss, and nail clubbing. Complications may include pulmonary hypertension, respiratory failure, pneumothorax, and lung cancer.

Pneumonitis describes general inflammation of lung tissue. Possible causative agents include radiation therapy of the chest, exposure to medications used during chemo-therapy, the inhalation of debris, aspiration, herbicides or fluorocarbons and some systemic diseases. If unresolved, continued inflammation can result in irreparable damage such as pulmonary fibrosis.

Cryptogenic organizing pneumonia (COP), formerly known as bronchiolitis obliterans organizing pneumonia (BOOP), is an inflammation of the bronchioles (bronchiolitis) and surrounding tissue in the lungs. It is a form of idiopathic interstitial pneumonia.
Lymphoproliferative disorders (LPDs) refer to a specific class of diagnoses, comprising a group of several conditions, in which lymphocytes are produced in excessive quantities. These disorders primarily present in patients who have a compromised immune system. Due to this factor, there are instances of these conditions being equated with "immunoproliferative disorders"; although, in terms of nomenclature, lymphoproliferative disorders are a subclass of immunoproliferative disorders—along with hypergammaglobulinemia and paraproteinemias.

Neurosyphilis refers to infection of the central nervous system in a patient with syphilis. In the era of modern antibiotics the majority of neurosyphilis cases have been reported in HIV-infected patients. Meningitis is the most common neurological presentation in early syphilis. Tertiary syphilis symptoms are exclusively neurosyphilis, though neurosyphilis may occur at any stage of infection.
Autoimmune hemolytic anemia (AIHA) occurs when antibodies directed against the person's own red blood cells (RBCs) cause them to burst (lyse), leading to an insufficient number of oxygen-carrying red blood cells in the circulation. The lifetime of the RBCs is reduced from the normal 100–120 days to just a few days in serious cases. The intracellular components of the RBCs are released into the circulating blood and into tissues, leading to some of the characteristic symptoms of this condition. The antibodies are usually directed against high-incidence antigens, therefore they also commonly act on allogenic RBCs. AIHA is a relatively rare condition, with an incidence of 5-10 cases per 1 million persons per year in the warm-antibody type and 0.45 to 1.9 cases per 1 million persons per year in the cold antibody type. Autoimmune hemolysis might be a precursor of later onset systemic lupus erythematosus.
Fever of unknown origin (FUO) refers to a condition in which the patient has an elevated temperature (fever) but, despite investigations by a physician, no explanation has been found.
Large granular lymphocytic (LGL) leukemia is a chronic lymphoproliferative disorder that exhibits an unexplained, chronic elevation in large granular lymphocytes (LGLs) in the peripheral blood.
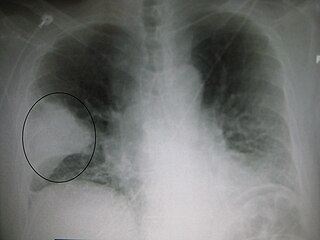
Pneumonia can be classified in several ways, most commonly by where it was acquired, but may also by the area of lung affected or by the causative organism. There is also a combined clinical classification, which combines factors such as age, risk factors for certain microorganisms, the presence of underlying lung disease or systemic disease and whether the person has recently been hospitalized.

The stages of HIV infection are acute infection, latency and AIDS. Acute infection lasts for several weeks and may include symptoms such as fever, swollen lymph nodes, inflammation of the throat, rash, muscle pain, malaise, and mouth and esophageal sores. The latency stage involves few or no symptoms and can last anywhere from two weeks to twenty years or more, depending on the individual. AIDS, the final stage of HIV infection, is defined by low CD4+ T cell counts, various opportunistic infections, cancers and other conditions.

Flock worker's lung is an occupational lung disease caused by exposure to flock, small fibers that are glued to a backing in order to create a specific texture. People who work in flocking are at risk of inhaling small pieces of the flock fibers, which causes interstitial lung disease. The disease was initially described in 1998, when a group of workers at a flocking plant developed interstitial lung disease of unknown cause.
Granulomatous–lymphocytic interstitial lung disease (GLILD) is a lung complication of common variable immunodeficiency disorders (CVID). It is seen in approximately 15% of patients with CVID. It has been defined histologically as the presence of (non-caseating) granuloma and lymphoproliferation in the lung. However, as GLILD is often associated with other auto-immune features such as splenomegaly, adenopathy and cytopenias, a definition based on abnormalities on lung imaging together with evidence of granulomatous inflammation elsewhere has also been employed.

Idiopathic multicentric Castleman disease (iMCD) is a subtype of Castleman disease, a group of lymphoproliferative disorders characterized by lymph node enlargement, characteristic features on microscopic analysis of enlarged lymph node tissue, and a range of symptoms and clinical findings.
Epstein–Barr virus–associated lymphoproliferative diseases are a group of disorders in which one or more types of lymphoid cells, i.e. B cells, T cells, NK cells, and histiocytic-dendritic cells, are infected with the Epstein–Barr virus (EBV). This causes the infected cells to divide excessively, and is associated with the development of various non-cancerous, pre-cancerous, and cancerous lymphoproliferative disorders (LPDs). These LPDs include the well-known disorder occurring during the initial infection with the EBV, infectious mononucleosis, and the large number of subsequent disorders that may occur thereafter. The virus is usually involved in the development and/or progression of these LPDs although in some cases it may be an "innocent" bystander, i.e. present in, but not contributing to, the disease.