Human teeth function to mechanically break down items of food by cutting and crushing them in preparation for swallowing and digesting. As such, they are considered part of the human digestive system. Humans have four types of teeth: incisors, canines, premolars, and molars, which each have a specific function. The incisors cut the food, the canines tear the food and the molars and premolars crush the food. The roots of teeth are embedded in the maxilla or the mandible and are covered by gums. Teeth are made of multiple tissues of varying density and hardness.

Toothache, also known as dental pain or tooth pain, is pain in the teeth or their supporting structures, caused by dental diseases or pain referred to the teeth by non-dental diseases. When severe it may impact sleep, eating, and other daily activities.

The pulp is the connective tissue, nerves, blood vessels, and odontoblasts that comprise the innermost layer of a tooth. The pulp's activity and signalling processes regulate its behaviour.

The periodontal ligament, commonly abbreviated as the PDL, are a group of specialized connective tissue fibers that essentially attach a tooth to the alveolar bone within which they sit. It inserts into root cementum on one side and onto alveolar bone on the other.

The dental follicle, also known as dental sac, is made up of mesenchymal cells and fibres surrounding the enamel organ and dental papilla of a developing tooth. It is a vascular fibrous sac containing the developing tooth and its odontogenic organ. The dental follicle (DF) differentiates into the periodontal ligament. In addition, it may be the precursor of other cells of the periodontium, including osteoblasts, cementoblasts and fibroblasts. They develop into the alveolar bone, the cementum with Sharpey's fibers and the periodontal ligament fibers respectively. Similar to dental papilla, the dental follicle provides nutrition to the enamel organ and dental papilla and also have an extremely rich blood supply.

A dentigerous cyst, also known as a follicular cyst, is an epithelial-lined developmental cyst formed by accumulation of fluid between the reduced enamel epithelium and the crown of an unerupted tooth. It is formed when there is an alteration in the reduced enamel epithelium and encloses the crown of an unerupted tooth at the cemento-enamel junction. Fluid is accumulated between reduced enamel epithelium and the crown of an unerupted tooth.
Dens invaginatus (DI), also known as tooth within a tooth, is a rare dental malformation and a developmental anomaly where there is an infolding of enamel into dentin. The prevalence of this condition is 0.3 - 10%, affecting males more frequently than females. The condition presents in two forms, coronal involving tooth crown and radicular involving tooth root, with the former being more common.
Dens evaginatus is a rare odontogenic developmental anomaly that is found in teeth where the outer surface appears to form an extra bump or cusp.

An odontogenic keratocyst is a rare and benign but locally aggressive developmental cyst. It most often affects the posterior mandible and most commonly presents in the third decade of life. Odontogenic keratocysts make up around 19% of jaw cysts. Despite its more common appearance in the bone region, it can affect soft tissue.
“Lateral periodontal cysts (LPCs) are defined as non-keratinised and non-inflammatory developmental cysts located adjacent or lateral to the root of a vital tooth.” LPCs are a rare form of jaw cysts, with the same histopathological characteristics as gingival cysts of adults (GCA). Hence LPCs are regarded as the intraosseous form of the extraosseous GCA. They are commonly found along the lateral periodontium or within the bone between the roots of vital teeth, around mandibular canines and premolars. Standish and Shafer reported the first well-documented case of LPCs in 1958, followed by Holder and Kunkel in the same year although it was called a periodontal cyst. Since then, there has been more than 270 well-documented cases of LPCs in literature.

Calcifying odontogenic cyst (COC) is a rare developmental lesion that comes from odontogenic epithelium. It is also known as a calcifying cystic odontogenic tumor, which is a proliferation of odontogenic epithelium and scattered nest of ghost cells and calcifications that may form the lining of a cyst, or present as a solid mass.

A dental abscess is a localized collection of pus associated with a tooth. The most common type of dental abscess is a periapical abscess, and the second most common is a periodontal abscess. In a periapical abscess, usually the origin is a bacterial infection that has accumulated in the soft, often dead, pulp of the tooth. This can be caused by tooth decay, broken teeth or extensive periodontal disease. A failed root canal treatment may also create a similar abscess.
Apical periodontitis is typically the body's defense response to the threat of microbial invasion from the root canal. Primary among the members of the host defense mechanism is the polymorphonuclear leukocyte, otherwise known as the neutrophil. The task of the neutrophil is to locate and destroy microbes that intrude into the body – anywhere in the body – and they represent the hallmark of acute inflammation.
Dental pertains to the teeth, including dentistry. Topics related to the dentistry, the human mouth and teeth include:

Resorption of the root of the tooth, or root resorption, is the progressive loss of dentin and cementum by the action of odontoclasts. Root resorption is a normal physiological process that occurs in the exfoliation of the primary dentition. However, pathological root resorption occurs in the permanent or secondary dentition and sometimes in the primary dentition.
Pulp necrosis is a clinical diagnostic category indicating the death of cells and tissues in the pulp chamber of a tooth with or without bacterial invasion. It is often the result of many cases of dental trauma, caries and irreversible pulpitis.
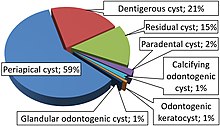
Odontogenic cysts are a group of jaw cysts that are formed from tissues involved in odontogenesis. Odontogenic cysts are closed sacs, and have a distinct membrane derived from the rest of odontogenic epithelium. It may contain air, fluids, or semi-solid material. Intra-bony cysts are most common in the jaws, because the mandible and maxilla are the only bones with epithelial components. That odontogenic epithelium is critical in normal tooth development. However, epithelial rests may be the origin for the cyst lining later. Not all oral cysts are odontogenic cysts. For example, mucous cyst of the oral mucosa and nasolabial duct cyst are not of odontogenic origin.
Cysts of the jaws are cysts—pathological epithelial-lined cavities filled with fluid or soft material—occurring on the bones of the jaws, the mandible and maxilla. Those are the bones with the highest prevalence of cysts in the human body, due to the abundant amount of epithelial remnants that can be left in the bones of the jaws. The enamel of teeth is formed from ectoderm, and so remnants of epithelium can be left in the bone during odontogenesis. The bones of the jaws develop from embryologic processes which fuse, and ectodermal tissue may be trapped along the lines of this fusion. This "resting" epithelium is usually dormant or undergoes atrophy, but, when stimulated, may form a cyst. The reasons why resting epithelium may proliferate and undergo cystic transformation are generally unknown, but inflammation is thought to be a major factor. The high prevalence of tooth impactions and dental infections that occur in the bones of the jaws is also significant to explain why cysts are more common at these sites.

Periapical periodontitis or apical periodontitis (AP) is an acute or chronic inflammatory lesion around the apex of a tooth root, most commonly caused by bacterial invasion of the pulp of the tooth. It is a likely outcome of untreated dental caries, and in such cases it can be considered a sequela in the natural history of tooth decay, irreversible pulpitis and pulpal necrosis. Other causes can include occlusal trauma due to 'high spots' after restoration work, extrusion from the tooth of root filling material, or bacterial invasion and infection from the gums. Periapical periodontitis may develop into a periapical abscess, where a collection of pus forms at the end of the root, the consequence of spread of infection from the tooth pulp, or into a periapical cyst, where an epithelial lined, fluid-filled structure forms.
Periapical granuloma, also sometimes referred to as a radicular granuloma or apical granuloma, is an inflammation at the tip of a dead (nonvital) tooth. It is a lesion or mass that typically starts out as an epithelial lined cyst, and undergoes an inward curvature that results in inflammation of granulation tissue at the root tips of a dead tooth. This is usually due to dental caries or a bacterial infection of the dental pulp. Periapical granuloma is an infrequent disorder that has an occurrence rate between 9.3 to 87.1 percent. Periapical granuloma is not a true granuloma due to the fact that it does not contain granulomatous inflammation; however, periapical granuloma is a common term used.