Cutaneous squamous-cell carcinoma (cSCC), or squamous-cell carcinoma of the skin, also known as squamous-cell skin cancer, is, with basal-cell carcinoma and melanoma, one of the three principal types of skin cancer. cSCC typically presents as a hard lump with a scaly top layer, but it may instead form an ulcer. Onset often occurs over a period of months. Cutaneous squamous-cell carcinoma is more likely to spread to distant areas than basal cell cancer. When confined to the outermost layer of the skin, a pre-invasive, or in situ, form of cSCC is known as Bowen's disease.

A sebaceous gland or oil gland is a microscopic exocrine gland in the skin that opens into a hair follicle to secrete an oily or waxy matter, called sebum, which lubricates the hair and skin of mammals. In humans, sebaceous glands occur in the greatest number on the face and scalp, but also on all parts of the skin except the palms of the hands and soles of the feet. In the eyelids, meibomian glands, also called tarsal glands, are a type of sebaceous gland that secrete a special type of sebum into tears. Surrounding the female nipple, areolar glands are specialized sebaceous glands for lubricating the nipple. Fordyce spots are benign, visible, sebaceous glands found usually on the lips, gums and inner cheeks, and genitals.

The scalp is the area of the head where head hair grows. It is made up of skin, layers of connective and fibrous tissues, and the membrane of the skull. Anatomically, the scalp is part of the epicranium, a collection of structures covering the cranium. The scalp is bordered by the face at the front, and by the neck at the sides and back. The scientific study of hair and scalp is called trichology.

Basal-cell carcinoma (BCC), also known as basal-cell cancer, basalioma or rodent ulcer, is the most common type of skin cancer. It often appears as a painless raised area of skin, which may be shiny with small blood vessels running over it. It may also present as a raised area with ulceration. Basal-cell cancer grows slowly and can damage the tissue around it, but it is unlikely to spread to distant areas or result in death.

A sebaceous cyst is a term commonly used to refer to either:

An epidermoid cyst or epidermal inclusion cyst is a benign cyst usually found on the skin. The cyst develops out of ectodermal tissue. Histologically, it is made of a thin layer of squamous epithelium.

Actinic keratosis (AK), sometimes called solar keratosis or senile keratosis, is a pre-cancerous area of thick, scaly, or crusty skin. Actinic keratosis is a disorder of epidermal keratinocytes that is induced by ultraviolet (UV) light exposure. These growths are more common in fair-skinned people and those who are frequently in the sun. They are believed to form when skin gets damaged by UV radiation from the sun or indoor tanning beds, usually over the course of decades. Given their pre-cancerous nature, if left untreated, they may turn into a type of skin cancer called squamous cell carcinoma. Untreated lesions have up to a 20% risk of progression to squamous cell carcinoma, so treatment by a dermatologist is recommended.

Birt–Hogg–Dubé syndrome (BHD), also Hornstein–Birt–Hogg–Dubé syndrome, Hornstein–Knickenberg syndrome, and fibrofolliculomas with trichodiscomas and acrochordons is a human, adult onset, autosomal dominant genetic disorder caused by the FLCN gene. It can cause susceptibility to kidney cancer, renal and pulmonary cysts, and noncancerous tumors of the hair follicles, called fibrofolliculomas. The symptoms seen in each family are unique, and can include any combination of the three symptoms. Fibrofolliculomas are the most common manifestation, found on the face and upper trunk in over 80% of people with BHD over the age of 40. Pulmonary cysts are equally common (84%) and 24% of people with BHD eventually experience a collapsed lung. Kidney tumors, both cancerous and benign, occur in 14–34% of people with BHD; the associated kidney cancers are often rare hybrid tumors.

Fordyce spots are harmless and painless visible sebaceous glands typically appearing as white/yellow small bumps or spots on the inside of lips or cheeks, gums, or genitalia. They are common, and are present in around 80% of adults. Treatment is generally not required and attempts to remove them typically result in pain and scarring.

Keratoacanthoma (KA) is a common low-grade rapidly-growing skin tumour that is believed to originate from the hair follicle and can resemble squamous cell carcinoma.

Mohs surgery, developed in 1938 by a general surgeon, Frederic E. Mohs, is microscopically controlled surgery used to treat both common and rare types of skin cancer. During the surgery, after each removal of tissue and while the patient waits, the tissue is examined for cancer cells. That examination dictates the decision for additional tissue removal. Mohs surgery is the gold standard method for obtaining complete margin control during removal of a skin cancer using frozen section histology. CCPDMA or Mohs surgery allows for the removal of a skin cancer with very narrow surgical margin and a high cure rate.

Verrucous carcinoma (VC) is an uncommon variant of squamous cell carcinoma. This form of cancer is often seen in those who chew tobacco or use snuff orally, so much so that it is sometimes referred to as "Snuff dipper's cancer".

Skin biopsy is a biopsy technique in which a skin lesion is removed to be sent to a pathologist to render a microscopic diagnosis. It is usually done under local anesthetic in a physician's office, and results are often available in 4 to 10 days. It is commonly performed by dermatologists. Skin biopsies are also done by family physicians, internists, surgeons, and other specialties. However, performed incorrectly, and without appropriate clinical information, a pathologist's interpretation of a skin biopsy can be severely limited, and therefore doctors and patients may forgo traditional biopsy techniques and instead choose Mohs surgery.
Sebaceous carcinoma, also known as sebaceous gland carcinoma (SGc), sebaceous cell carcinoma, and meibomian gland carcinoma is an uncommon malignant cutaneous tumor. Most are typically about 1.4 cm at presentation. SGc originates from sebaceous glands in the skin and, therefore, may originate anywhere in the body where these glands are found. SGc can be divided into 2 types: periocular and extraocular. The periocular region is rich in sebaceous glands making it a common site of origin. The cause of these lesions in the vast majority of cases is unknown. Occasional cases may be associated with Muir-Torre syndrome. SGc accounts for approximately 0.7% of all skin cancers, and the incidence of SGc is highest in Caucasian, Asian, and Indian populations. Due to the rarity of this tumor and variability in clinical and histological presentation, SGc is often misdiagnosed as an inflammatory condition or a more common neoplasm. SGc is commonly treated with wide local excision or Mohs micrographic surgery, and the relative survival rates at 5 and 10 years are 92.72 and 86.98%, respectively.

Syringocystadenoma papilliferum is a rare non-malignant adnexal neoplasm that develops from apocrine or eccrine sweat glands and can be identified histologically by cystic, papillary, and ductal invaginations into the dermis lined by double-layered outer cuboidal and luminal high columnar epithelium and connected to the epidermis.
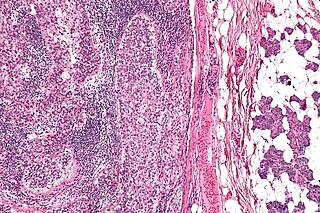
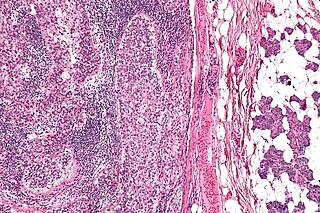
Cock's peculiar tumour is a sebaceous cyst linked growth that can resemble a squamous cell carcinoma. The name is given after a 19th-century English surgeon Edward Cock. The proliferating cyst is usually solitary, but it often arises from a simple trichilemmal cysts in the hair follicle epithelium and these are multiple in 70% of cases. They are most commonly found on the scalp where the proliferating trichilemmal cyst will grow to a large size and ulcerate. Chronic inflammation can cause the cyst to take the form of a granuloma. This granuloma mimics a squamous-cell carcinoma and these ulcerating solitary cysts are called Cock's peculiar tumour.

Spiradenomas (SA) are rare, benign cutaneous adnexal tumors that may progress to become their malignant counterparts, i.e. spiradenocarcinomas (SAC). Cutaneous adnexal tumors are a group of skin tumors consisting of tissues that have differentiated towards one of the four primary adnexal structures found in normal skin: hair follicles, sebaceous sweat glands, apocrine sweat glands, and eccrine sweat glands. SA and SAC tumors were regarded as eccrine gland tumors and termed eccrine spiradenomas and eccrine spiradenocarcinomas, respectively. However, more recent studies have found them to be hair follicle tumors and commonly term them spiradenomas and spiradenocarcinomas, respectively. Further confusing the situation, SA-like and SAC-like tumors are also 1) manifestations of the inherited disorder, CYLD cutaneous syndrome (CCS), and 2) have repeatedly been confused with an entirely different tumor, adenoid cystic carcinomas of the salivary gland. Here, SA and SAC are strictly defined as sporadic hair follicle tumors that do not include the hereditary CCS spiradenomas and heridtary spiradenocarcinoms of CCS or the adenoid cystic carcinomas.

Proliferating trichilemmal cysts are a cutaneous condition characterized by proliferations of squamous cells forming scroll-like structures.
CYLD cutaneous syndrome (CCS) is the recently designated term for three rare inherited cutaneous adnexal tumor syndromes: multiple familial trichoepithelioma (MFT1), Brooke–Spiegler syndrome (BSS), and familial cylindromatosis (FC). Cutaneous adnexal tumors are a large group of skin tumors that consist of tissues that have differentiated towards one of the four primary adnexal structures found in normal skin: hair follicles, sebaceous sweat glands, apocrine sweat glands, and eccrine sweat glands. CCS tumors are hair follicle tumors.