A third molar, commonly called wisdom tooth, is one of the three molars per quadrant of the human dentition. It is the most posterior of the three. The age at which wisdom teeth come through (erupt) is variable, but this generally occurs between late teens and early twenties. Most adults have four wisdom teeth, one in each of the four quadrants, but it is possible to have none, fewer, or more, in which case the extras are called supernumerary teeth. Wisdom teeth may get stuck (impacted) against other teeth if there is not enough space for them to come through normally. Impacted wisdom teeth are still sometimes removed for orthodontic treatment, believing that they move the other teeth and cause crowding, though this is not held anymore as true. Impacted wisdom teeth may suffer from tooth decay if oral hygiene becomes more difficult. Wisdom teeth which are partially erupted through the gum may also cause inflammation and infection in the surrounding gum tissues, termed pericoronitis. Some more conservative treatments, such as operculectomies, may be fitting for some cases, yet impacted wisdom teeth are commonly extracted as treatment for these problems, many times before these problems, which might never happen, even occur. Some oppose this prophylactic removal of disease-free impacted wisdom teeth, including among them the National Institute for Health and Care Excellence in the UK.

Ameloblastoma is a rare, benign or cancerous tumor of odontogenic epithelium much more commonly appearing in the lower jaw than the upper jaw. It was recognized in 1827 by Cusack. This type of odontogenic neoplasm was designated as an adamantinoma in 1885 by the French physician Louis-Charles Malassez. It was finally renamed to the modern name ameloblastoma in 1930 by Ivey and Churchill.

Cementoblastoma, or benign cementoblastoma, is a relatively rare benign neoplasm of the cementum of the teeth. It is derived from ectomesenchyme of odontogenic origin. Cementoblastomas represent less than 0.69–8% of all odontogenic tumors.

The dental follicle, also known as dental sac, is made up of mesenchymal cells and fibres surrounding the enamel organ and dental papilla of a developing tooth. It is a vascular fibrous sac containing the developing tooth and its odontogenic organ. The dental follicle (DF) differentiates into the periodontal ligament. In addition, it may be the precursor of other cells of the periodontium, including osteoblasts, cementoblasts and fibroblasts. They develop into the alveolar bone, the cementum with Sharpey's fibers and the periodontal ligament fibers respectively. Similar to dental papilla, the dental follicle provides nutrition to the enamel organ and dental papilla and also have an extremely rich blood supply.

Veterinary dentistry is the field of dentistry applied to the care of animals. It is the art and science of prevention, diagnosis, and treatment of conditions, diseases, and disorders of the oral cavity, the maxillofacial region, and its associated structures as it relates to animals.

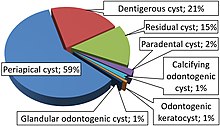
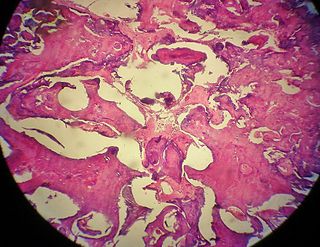
Dentigerous cyst, also known as follicular cyst is an epithelial-lined developmental cyst formed by accumulation of fluid between the reduced enamel epithelium and crown of an unerupted tooth. It is formed when there is an alteration in the reduced enamel epithelium and encloses the crown of an unerupted tooth at the cemento-enamel junction. Fluid is accumulated between reduced enamel epithelium and the crown of an unerupted tooth. Dentigerous cyst is the second most common form of benign developmental odontogenic cysts.

Central giant-cell granuloma (CGCG) is a localised benign condition of the jaws. It is twice as common in females and is more likely to occur before age 30. Central giant-cell granulomas are more common in the anterior mandible, often crossing the midline and causing painless swellings.

Commonly known as a dental cyst, the periapical cyst is the most common odontogenic cyst. It may develop rapidly from a periapical granuloma, as a consequence of untreated chronic periapical periodontitis.

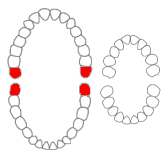
An odontogenic keratocyst is a rare and benign but locally aggressive developmental cyst. It most often affects the posterior mandible and most commonly presents in the third decade of life. Odontogenic keratocysts make up around 19% of jaw cysts.
“Lateral periodontal cysts (LPCs) are defined as non-keratinised and non-inflammatory developmental cysts located adjacent or lateral to the root of a vital tooth.” LPCs are a rare form of jaw cysts, with the same histopathological characteristics as gingival cysts of adults (GCA). Hence LPCs are regarded as the intraosseous form of the extraosseous GCA. They are commonly found along the lateral periodontium or within the bone between the roots of vital teeth, around mandibular canines and premolars. Standish and Shafer reported the first well-documented case of LPCs in 1958, followed by Holder and Kunkel in the same year although it was called a periodontal cyst. Since then, there has been more than 270 well-documented cases of LPCs in literature.

Calcifying odotogenic cyst (COC) is a rare developmental lesion that comes from odontogenic epithelium. It is also known as a calcifying cystic odontogenic tumor, which is a proliferation of odontogenic epithelium and scattered nest of ghost cells and calcifications that may form the lining of a cyst, or present as a solid mass.

A glandular odontogenic cyst (GOC) is a rare and usually benign odontogenic cyst developed at the odontogenic epithelium of the mandible or maxilla. Originally, the cyst was labeled as "sialo-odontogenic cyst" in 1987. However, the World Health Organization (WHO) decided to adopt the medical expression "glandular odontogenic cyst". Following the initial classification, only 60 medically documented cases were present in the population by 2003. GOC was established as its own biological growth after differentiation from other jaw cysts such as the "central mucoepidermoid carcinoma (MEC)", a popular type of neoplasm at the salivary glands. GOC is usually misdiagnosed with other lesions developed at the glandular and salivary gland due to the shared clinical signs. The presence of osteodentin supports the concept of an odontogenic pathway. This odontogenic cyst is commonly described to be a slow and aggressive development. The inclination of GOC to be large and multilocular is associated with a greater chance of remission. GOC is an infrequent manifestation with a 0.2% diagnosis in jaw lesion cases. Reported cases show that GOC mainly impacts the mandible and male individuals. The presentation of GOC at the maxilla has a very low rate of incidence. The GOC development is more common in adults in their fifth and sixth decades.

The adenomatoid odontogenic tumor is an odontogenic tumor arising from the enamel organ or dental lamina.
Squamous odontogenic tumors (SOTs) are very rare benign locally infiltrative odontogenic neoplasms of epithelial origin. Only some 50 cases have been documented. They occur mostly from 20-40 and are more common in males. Treatment is by simple enucleation and local curettage, and recurrence is rare.
An ameloblastic fibroma is a fibroma of the ameloblastic tissue, that is, an odontogenic tumor arising from the enamel organ or dental lamina. It may be either truly neoplastic or merely hamartomatous. In neoplastic cases, it may be labeled an ameloblastic fibrosarcoma in accord with the terminological distinction that reserves the word fibroma for benign tumors and assigns the word fibrosarcoma to malignant ones. It is more common in the first and second decades of life, when odontogenesis is ongoing, than in later decades. In 50% of cases an unerupted tooth is involved.
An odontoma, also known as an odontome, is a benign tumour linked to tooth development. Specifically, it is a dental hamartoma, meaning that it is composed of normal dental tissue that has grown in an irregular way. It includes both odontogenic hard and soft tissues. As with normal tooth development, odontomas stop growing once mature which makes them benign.
The odontogenic myxoma is an uncommon benign odontogenic tumor arising from embryonic connective tissue associated with tooth formation. As a myxoma, this tumor consists mainly of spindle shaped cells and scattered collagen fibers distributed through a loose, mucoid material.

A bone cyst or geode is a cyst that forms in bone.
Odontogenic cyst are a group of jaw cysts that are formed from tissues involved in odontogenesis. Odontogenic cysts are closed sacs, and have a distinct membrane derived from rests of odontogenic epithelium. It may contain air, fluids, or semi-solid material. Intra-bony cysts are most common in the jaws, because the mandible and maxilla are the only bones with epithelial components. That odontogenic epithelium is critical in normal tooth development. However, epithelial rests may be the origin for the cyst lining later. Not all oral cysts are odontogenic cyst. For example, mucous cyst of the oral mucosa and nasolabial duct cyst are not of odontogenic origin.
In addition, there are several conditions with so-called (radiographic) 'pseudocystic appearance' in jaws; ranging from anatomic variants such as Stafne static bone cyst, to the aggressive aneurysmal bone cyst.

Gingival cyst, also known as Epstein's pearl, is a type of cysts of the jaws that originates from the dental lamina and is found in the mouth parts. It is a superficial cyst in the alveolar mucosa. It can be seen inside the mouth as small and whitish bulge. Depending on the ages in which they develop, the cysts are classified into gingival cyst of newborn and gingival cyst of adult. Structurally, the cyst is lined by thin epithelium and shows a lumen usually filled with desquamated keratin, occasionally containing inflammatory cells. The nodes are formed as a result of cystic degeneration of epithelial rests of the dental lamina.