A mouth ulcer (aphtha) is an ulcer that occurs on the mucous membrane of the oral cavity. Mouth ulcers are very common, occurring in association with many diseases and by many different mechanisms, but usually there is no serious underlying cause. Rarely, a mouth ulcer that does not heal may be a sign of oral cancer. These ulcers may form individually or multiple ulcers may appear at once. Once formed, an ulcer may be maintained by inflammation and/or secondary infection.

A granuloma is an aggregation of macrophages that forms in response to chronic inflammation. This occurs when the immune system attempts to isolate foreign substances that it is otherwise unable to eliminate. Such substances include infectious organisms including bacteria and fungi, as well as other materials such as foreign objects, keratin, and suture fragments.

Granulomatosis with polyangiitis (GPA), previously known as Wegener's granulomatosis (WG), is a rare long-term systemic disorder that involves the formation of granulomas and inflammation of blood vessels (vasculitis). It is a form of vasculitis that affects small- and medium-size vessels in many organs but most commonly affects the upper respiratory tract, lungs and kidneys. The signs and symptoms of GPA are highly varied and reflect which organs are supplied by the affected blood vessels. Typical signs and symptoms include nosebleeds, stuffy nose and crustiness of nasal secretions, and inflammation of the uveal layer of the eye. Damage to the heart, lungs and kidneys can be fatal.

Uveitis is the inflammation of the uvea, the pigmented layer that lies between the inner retina and the outer fibrous layer composed of the sclera and cornea. The uvea consists of the middle layer of pigmented vascular structures of the eye and includes the iris, ciliary body, and choroid. Uveitis is described anatomically, by the part of the eye affected, as anterior, intermediate or posterior, from front to back. In the panuveitic form, all parts are involved. The commonest is the anterior form. Symptoms include pain, floaters and blurred vision, and clinical examination may show redness and an irregular pupil, while opthalmic examination shows dilated ciliary blood vessels and the presence of cells in the anterior chamber. Uveitis may arise spontaneously and associated with some genetic factors, or be associated with a wide range of conditions including autoimmune disease and infections. While the eye is a relatively protected environment, its immune mechanisms may be overcome resulting in inflammation and tissue destruction associated with T-cell activation. The incidence is approximately 1:4500, most commonly between the ages of 20–60.

Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the oesophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.

Tuberculous lymphadenitis is the most common form of tuberculosis infections that appears outside the lungs. Tuberculous lymphadenitis is a chronic, specific granulomatous inflammation of the lymph node with caseation necrosis, caused by infection with Mycobacterium tuberculosis or related bacteria.

Stomatitis is inflammation of the mouth and lips. It refers to any inflammatory process affecting the mucous membranes of the mouth and lips, with or without oral ulceration.

Angular cheilitis (AC) is inflammation of one or both corners of the mouth. Often the corners are red with skin breakdown and crusting. It can also be itchy or painful. The condition can last for days to years. Angular cheilitis is a type of cheilitis.

Melkersson–Rosenthal syndrome is a rare neurological disorder characterized by recurring facial paralysis, swelling of the face and lips and the development of folds and furrows in the tongue. Onset is in childhood or early adolescence. After recurrent attacks, swelling may persist and increase, eventually becoming permanent. The lip may become hard, cracked, and fissured with a reddish-brown discoloration. The cause of Melkersson–Rosenthal syndrome is unknown, but there may be a genetic predisposition. It has been noted to be especially prevalent among certain ethnic groups in Bolivia. It can be symptomatic of Crohn's disease or sarcoidosis. Approximately 400 cases have been reported worldwide.
An oral medicine or stomatology doctor has received additional specialized training and experience in the diagnosis and management of oral mucosal abnormalities including oral cancer, salivary gland disorders, temporomandibular disorders and facial pain, taste and smell disorders; and recognition of the oral manifestations of systemic and infectious diseases. It lies at the interface between medicine and dentistry. An oral medicine doctor is trained to diagnose and manage patients with disorders of the orofacial region, essentially as a "physician of the mouth."

Sialadenitis (sialoadenitis) is inflammation of salivary glands, usually the major ones, the most common being the parotid gland, followed by submandibular and sublingual glands. It should not be confused with sialadenosis (sialosis) which is a non-inflammatory enlargement of the major salivary glands.

Cheilitis is a medical condition characterized by inflammation of the lips. According to its onset and course, cheilitis can be either acute or chronic. Most cheilitis is caused by acute sun exposure. Allergic tests may identify allergens that cause cheilitis.

Gingival enlargement is an increase in the size of the gingiva (gums). It is a common feature of gingival disease. Gingival enlargement can be caused by a number of factors, including inflammatory conditions and the side effects of certain medications. The treatment is based on the cause. A closely related term is epulis, denoting a localized tumor on the gingiva.
Oral and maxillofacial pathology refers to the diseases of the mouth, jaws and related structures such as salivary glands, temporomandibular joints, facial muscles and perioral skin. The mouth is an important organ with many different functions. It is also prone to a variety of medical and dental disorders.
Persistent edema of rosacea is a hard, nonpitting edema found on the areas involved, those mainly being the forehead, glabella, upper eyelids, nose, and/or cheeks.

Blau Syndrome is an autosomal dominant genetic inflammatory disorder which affects the skin, eyes, and joints. It is caused by a mutation in the NOD2 (CARD15) gene. Symptoms usually begin before the age of 4, and the disease manifests as early onset cutaneous sarcoidosis, granulomatous arthritis, and uveitis.

Plasma cell gingivitis is a rare condition, appearing as generalized erythema (redness) and edema (swelling) of the attached gingiva, occasionally accompanied by cheilitis or glossitis. It is called plasma cell gingivitis where the gingiva (gums) are involved, plasma cell cheilitis, where the lips are involved, and other terms such as plasma cell orifacial mucositis, or plasma cell gingivostomatitis where several sites in the mouth are involved. On the lips, the condition appears as sharply outlined, infiltrated, dark red plaque with a lacquer-like glazing of the surface of the involved oral area.

Cervical lymphadenopathy refers to lymphadenopathy of the cervical lymph nodes. The term lymphadenopathy strictly speaking refers to disease of the lymph nodes, though it is often used to describe the enlargement of the lymph nodes. Similarly, the term lymphadenitis refers to inflammation of a lymph node, but often it is used as a synonym of lymphadenopathy.
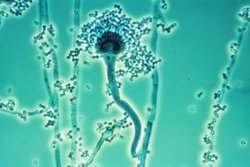
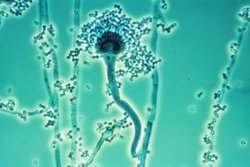
Fungal sinusitis is the inflammation of the lining mucosa of the paranasal sinuses due to fungal infection. It occurs in people with reduced immunity. The maxillary sinus is the most commonly involved. Fungi responsible for fungal sinusitis are Aspergillus fumigatus (90%), Aspergillus flavus, and Aspergillus niger. Fungal sinusitis occurs most commonly in middle-aged populations. Diabetes mellitus is the most common risk factor involved.
Oral manifestations of systematic disease are signs and symptoms of disease occurring elsewhere in the body detected in the oral cavity and oral secretions. High blood sugar can be detected by sampling saliva. Saliva sampling may be a non-invasive way to detect changes in the gut microbiome and changes in systemic disease. Another example is tertiary syphilis, where changes to teeth can occur. Syphilis infection can be associated with longitudinal furrows of the tongue.