The gums or gingiva consist of the mucosal tissue that lies over the mandible and maxilla inside the mouth. Gum health and disease can have an effect on general health.

Stomatitis is inflammation of the mouth and lips. It refers to any inflammatory process affecting the mucous membranes of the mouth and lips, with or without oral ulceration.
Periodontology or periodontics is the specialty of dentistry that studies supporting structures of teeth, as well as diseases and conditions that affect them. The supporting tissues are known as the periodontium, which includes the gingiva (gums), alveolar bone, cementum, and the periodontal ligament. A periodontist is a dentist that specializes in the prevention, diagnosis and treatment of periodontal disease and in the placement of dental implants.

Glossitis can mean soreness of the tongue, or more usually inflammation with depapillation of the dorsal surface of the tongue, leaving a smooth and erythematous (reddened) surface,. In a wider sense, glossitis can mean inflammation of the tongue generally. Glossitis is often caused by nutritional deficiencies and may be painless or cause discomfort. Glossitis usually responds well to treatment if the cause is identified and corrected. Tongue soreness caused by glossitis is differentiated from burning mouth syndrome, where there is no identifiable change in the appearance of the tongue, and there are no identifiable causes.

Angular cheilitis (AC) is inflammation of one or both corners of the mouth. Often the corners are red with skin breakdown and crusting. It can also be itchy or painful. The condition can last for days to years. Angular cheilitis is a type of cheilitis.

Veterinary dentistry is the field of dentistry applied to the care of animals. It is the art and science of prevention, diagnosis, and treatment of conditions, diseases, and disorders of the oral cavity, the maxillofacial region, and its associated structures as it relates to animals.

Gingival recession, also known as gum recession and receding gums, is the exposure in the roots of the teeth caused by a loss of gum tissue and/or retraction of the gingival margin from the crown of the teeth. Gum recession is a common problem in adults over the age of 40, but it may also occur starting in adolescence, or around the age of 10. It may exist with or without concomitant decrease in crown-to-root ratio.

Cheilitis is a medical condition characterized by inflammation of the lips. The inflammation may include the perioral skin, the vermilion border, or the labial mucosa. The skin and the vermilion border are more commonly involved, as the mucosa is less affected by inflammatory and allergic reactions.
Orofacial granulomatosis (OFG) is a condition characterized by persistent enlargement of the soft tissues of the mouth, lips and the area around the mouth on the face, causing in most cases extreme pain. The mechanism of the enlargement is granulomatous inflammation. The underlying cause of the condition is not completely understood, and there is disagreement as to how it relates to Crohn's disease and sarcoidosis.
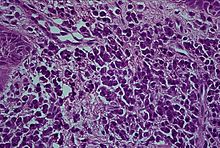
Desquamative gingivitis is an erythematous (red), desquamatous (shedding) and ulcerated appearance of the gums. It is a descriptive term and can be caused by several different disorders.

Scaling and root planing, also known as conventional periodontal therapy, non-surgical periodontal therapy or deep cleaning, is a procedure involving removal of dental plaque and calculus and then smoothing, or planing, of the (exposed) surfaces of the roots, removing cementum or dentine that is impregnated with calculus, toxins, or microorganisms, the agents that cause inflammation. It is a part of non-surgical periodontal therapy. This helps to establish a periodontium that is in remission of periodontal disease. Periodontal scalers and periodontal curettes are some of the tools involved.

Gingival enlargement is an increase in the size of the gingiva (gums). It is a common feature of gingival disease. Gingival enlargement can be caused by a number of factors, including inflammatory conditions and the side effects of certain medications. The treatment is based on the cause. A closely related term is epulis, denoting a localized tumor on the gingiva.
Dental pertains to the teeth, including dentistry. Topics related to the dentistry, the human mouth and teeth include:
Oral and maxillofacial pathology refers to the diseases of the mouth, jaws and related structures such as salivary glands, temporomandibular joints, facial muscles and perioral skin. The mouth is an important organ with many different functions. It is also prone to a variety of medical and dental disorders.

Gingivitis is a non-destructive disease that causes inflammation of the gums; ulitis is an alternative term. The most common form of gingivitis, and the most common form of periodontal disease overall, is in response to bacterial biofilms that are attached to tooth surfaces, termed plaque-induced gingivitis. Most forms of gingivitis are plaque-induced.
Epulis is any tumor like enlargement situated on the gingival or alveolar mucosa. The word literally means "(growth) on the gingiva", and describes only the location of the mass and has no further implications on the nature of the lesion. There are three types: fibromatous, ossifying and acanthomatous. The related term parulis refers to a mass of inflamed granulation tissue at the opening of a draining sinus on the alveolus over the root of an infected tooth. Another closely related term is gingival enlargement, which tends to be used where the enlargement is more generalized over the whole gingiva rather than a localized mass.

A periodontal abscess, is a localized collection of pus within the tissues of the periodontium. It is a type of dental abscess. A periodontal abscess occurs alongside a tooth, and is different from the more common periapical abscess, which represents the spread of infection from a dead tooth. To reflect this, sometimes the term "lateral (periodontal) abscess" is used. In contrast to a periapical abscess, periodontal abscesses are usually associated with a vital (living) tooth. Abscesses of the periodontium are acute bacterial infections classified primarily by location.
Gingivoplasty is the process by which the gingiva are reshaped to correct deformities. Gingivoplasty is similar to gingivectomy but with a different objective. This is a procedure performed to eliminate periodontal pockets along with the reshaping as part of the technique. This procedure is followed to create physiological gingival contours with the sole purpose of recontouring the gingiva in the absence of the pockets.
Hereditary gingival fibromatosis (HGF), also known as idiopathic gingival hyperplasia, is a rare condition of gingival overgrowth. HGF is characterized as a benign, slowly progressive, nonhemorrhagic, fibrous enlargement of keratinized gingiva. It can cover teeth in various degrees, and can lead to aesthetic disfigurement. Fibrous enlargement is most common in areas of maxillary and mandibular tissues of both arches in the mouth. Phenotype and genotype frequency of HGF is 1:175,000 where males and females are equally affected but the cause is not entirely known. It mainly exists as an isolated abnormality but can also be associated with a multi-system syndrome.