Stomatitis is inflammation of the mouth and lips. It refers to any inflammatory process affecting the mucous membranes of the mouth and lips, with or without oral ulceration.
The oral mucosa is the mucous membrane lining the inside of the mouth. It comprises stratified squamous epithelium, termed "oral epithelium", and an underlying connective tissue termed lamina propria. The oral cavity has sometimes been described as a mirror that reflects the health of the individual. Changes indicative of disease are seen as alterations in the oral mucosa lining the mouth, which can reveal systemic conditions, such as diabetes or vitamin deficiency, or the local effects of chronic tobacco or alcohol use. The oral mucosa tends to heal faster and with less scar formation compared to the skin. The underlying mechanism remains unknown, but research suggests that extracellular vesicles might be involved.
Epulis fissuratum is a benign hyperplasia of fibrous connective tissue which develops as a reactive lesion to chronic mechanical irritation produced by the flange of a poorly fitting denture. More simply, epulis fissuratum is where excess folds of firm tissue form inside the mouth, as a result of rubbing on the edge of dentures that do not fit well. It is a harmless condition and does not represent oral cancer. Treatment is by simple surgical removal of the lesion, and also by adjustment of the denture or provision of a new denture.
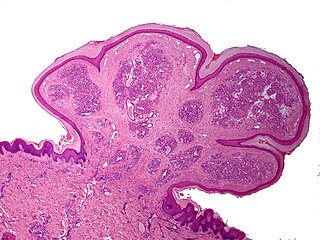
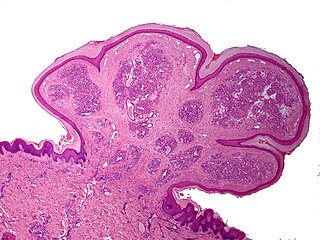
Inflammatory papillary hyperplasia (IPH) is a benign lesion of the oral mucosa which is characterized by the growth of one or more nodular lesions, measuring about 2mm or less. The lesion almost exclusively involves the hard palate, and in rare instances, it also has been seen on the mandible. The lesion is mostly asymptomatic and color of the mucosa may vary from pink to red.
A pyogenic granuloma or lobular capillary hemangioma is a vascular tumor that occurs on both mucosa and skin, and appears as an overgrowth of tissue due to irritation, physical trauma, or hormonal factors. It is often found to involve the gums, skin, or nasal septum, and has also been found far from the head, such as in the thigh.
Peripheral giant-cell granuloma (PGCG) is an oral pathologic condition that appears in the mouth as an overgrowth of tissue due to irritation or trauma. Because of its overwhelming incidence on the gingiva, the condition is associated with two other diseases, pyogenic granuloma and peripheral ossifying fibroma. These three diseases are associated because they appear frequently on gingiva. Due to its similar microscopic appearance, peripheral giant-cell granuloma is considered to be the soft tissue equivalent of central giant-cell granuloma.
A peripheral ossifying fibroma, also known as ossifying fibrous epulis, is “a gingival nodule which is composed of a cellular fibroblastic connective tissue stroma which is associated with the formation of randomly dispersed foci of mineralised products, which consists of bone, cementum-like tissue, or a dystrophic calcification. The lesion is considered part of an ossifying fibroma, but that is usually considered to be a jaw tumor. Because of its overwhelming incidence on the gingiva, the condition is associated with two other diseases, though not because they occur together. Instead, the three are associated with each other because they appear frequently on gingiva: pyogenic granuloma and peripheral giant cell granuloma. Some researchers believe peripheral ossifying fibromas to be related to pyogenic fibromas and, in some instances, are the result of a pyogenic granuloma which has undergone fibrosis and calcification.
An oral medicine or stomatology doctor/dentist has received additional specialized training and experience in the diagnosis and management of oral mucosal abnormalities including oral cancer, salivary gland disorders, temporomandibular disorders and facial pain, taste and smell disorders; and recognition of the oral manifestations of systemic and infectious diseases. It lies at the interface between medicine and dentistry. An oral medicine doctor is trained to diagnose and manage patients with disorders of the orofacial region.
Stomatitis nicotina is a diffuse white patch on the hard palate, usually caused by tobacco smoking, usually pipe or cigar smoking. It is painless, and it is caused by a response of the palatal oral mucosa to chronic heat. A more pronounced appearance can occur with reverse smoking, sometimes distinguished from stomatitis nicotina by the term reverse smoker's stomatitis. While stomatitis nicotina that is caused by heat is not a premalignant condition, the condition that is caused by reverse smoking is premalignant.
Giant-cell fibroma is a benign localized fibrous mass. It often mimics other fibroepithelial growths and can be distinguished by its histopathology. The exact cause of giant-cell fibromas is unknown however there is no evidence to show that it can be caused by irritation. Giant-cell fibromas can be removed by surgical incision, electrosurgery, or laser excision.
Orofacial granulomatosis (OFG) is a condition characterized by persistent enlargement of the soft tissues of the mouth, lips and the area around the mouth on the face, causing in most cases extreme pain. The mechanism of the enlargement is granulomatous inflammation. The underlying cause of the condition is not completely understood, and there is disagreement as to how it relates to Crohn's disease and sarcoidosis.

Central giant-cell granuloma (CGCG) is a localised benign condition of the jaws. It is twice as common in females and is more likely to occur before age 30. Central giant-cell granulomas are more common in the anterior mandible, often crossing the midline and causing painless swellings.

Calcifying odontogenic cyst (COC) is a rare developmental lesion that comes from odontogenic epithelium. It is also known as a calcifying cystic odontogenic tumor, which is a proliferation of odontogenic epithelium and scattered nest of ghost cells and calcifications that may form the lining of a cyst, or present as a solid mass.
Peripheral odontogenic fibroma(PFO) is a fibrous connective tissue mass that is exophytic and covered in surface epithelium that contains odontogenic epithelium. The World Health Organization (WHO) classifies peripheral odontogenic fibroma as a fibroblastic neoplasm with variable amounts of odontogenic epithelium that appears to be dormant. Dentine and/or cementum-like material may be present.

Gingival enlargement is an increase in the size of the gingiva (gums). It is a common feature of gingival disease. Gingival enlargement can be caused by a number of factors, including inflammatory conditions and the side effects of certain medications. The treatment is based on the cause. A closely related term is epulis, denoting a localized tumor on the gingiva.
Dental pertains to the teeth, including dentistry. Topics related to the dentistry, the human mouth and teeth include:

Plasma cell gingivitis is a rare condition, appearing as generalized erythema (redness) and edema (swelling) of the attached gingiva, occasionally accompanied by cheilitis or glossitis. It is called plasma cell gingivitis where the gingiva (gums) are involved, plasma cell cheilitis, where the lips are involved, and other terms such as plasma cell orifacial mucositis, or plasma cell gingivostomatitis where several sites in the mouth are involved. On the lips, the condition appears as sharply outlined, infiltrated, dark red plaque with a lacquer-like glazing of the surface of the involved oral area.
Cysts of the jaws are cysts—pathological epithelial-lined cavities filled with fluid or soft material—occurring on the bones of the jaws, the mandible and maxilla. Those are the bones with the highest prevalence of cysts in the human body, due to the abundant amount of epithelial remnants that can be left in the bones of the jaws. The enamel of teeth is formed from ectoderm, and so remnants of epithelium can be left in the bone during odontogenesis. The bones of the jaws develop from embryologic processes which fuse, and ectodermal tissue may be trapped along the lines of this fusion. This "resting" epithelium is usually dormant or undergoes atrophy, but, when stimulated, may form a cyst. The reasons why resting epithelium may proliferate and undergo cystic transformation are generally unknown, but inflammation is thought to be a major factor. The high prevalence of tooth impactions and dental infections that occur in the bones of the jaws is also significant to explain why cysts are more common at these sites.
Plasma cell granulomas (PCGs) are uncommon, non-neoplastic lesions of unknown etiology and are considered an entity of IgG4-related diseases.

Amalgam tattoo is a grey, blue or black area of discoloration on the mucous membranes of the mouth, typically on the gums of the lower jaw. It is a healthcare caused lesion, due to entry of dental amalgam into the soft tissues. It is common, painless, and benign, but it can be mistaken for melanoma.