The salivary glands in many vertebrates including mammals are exocrine glands that produce saliva through a system of ducts. Humans have three paired major salivary glands, as well as hundreds of minor salivary glands. Salivary glands can be classified as serous, mucous, or seromucous (mixed).

A mouth ulcer (aphtha) is an ulcer that occurs on the mucous membrane of the oral cavity. Mouth ulcers are very common, occurring in association with many diseases and by many different mechanisms, but usually there is no serious underlying cause. Rarely, a mouth ulcer that does not heal may be a sign of oral cancer. These ulcers may form individually or multiple ulcers may appear at once. Once formed, an ulcer may be maintained by inflammation and/or secondary infection.

Oral cancer, also known as mouth cancer, is a cancer of the lining of the lips, mouth, or upper throat. In the mouth, it most commonly starts as a painless white patch, that thickens, develops red patches, an ulcer, and continues to grow. When on the lips, it commonly looks like a persistent crusting ulcer that does not heal, and slowly grows. Other symptoms may include difficult or painful swallowing, new lumps or bumps in the neck, a swelling in the mouth, or a feeling of numbness in the mouth or lips.

Head and neck cancer develops from tissues in the lip and oral cavity (mouth), larynx (throat), salivary glands, nose, sinuses, or skin of the face. The most common types of head and neck cancer occur in the lips, mouth, and larynx. Symptoms predominantly include a sore that does not heal or a change in the voice. In those with advanced disease, there may be unusual bleeding, facial pain, numbness or swelling, and visible lumps on the outside of the neck or oral cavity. Given the location of these cancers, trouble breathing may also be present.

Oral leukoplakia is a potentially malignant disorder affecting the oral mucosa. It is defined as "essentially an oral mucosal white lesion that cannot be considered as any other definable lesion." Oral leukoplakia is a white patch or plaque that develops in the oral cavity and is strongly associated with smoking. Leukoplakia is a firmly attached white patch on a mucous membrane which is associated with increased risk of cancer. The edges of the lesion are typically abrupt and the lesion changes with time. Advanced forms may develop red patches. There are generally no other symptoms. It usually occurs within the mouth, although sometimes mucosa in other parts of the gastrointestinal tract, urinary tract, or genitals may be affected.
The oral mucosa is the mucous membrane lining the inside of the mouth. It comprises stratified squamous epithelium, termed "oral epithelium", and an underlying connective tissue termed lamina propria. The oral cavity has sometimes been described as a mirror that reflects the health of the individual. Changes indicative of disease are seen as alterations in the oral mucosa lining the mouth, which can reveal systemic conditions, such as diabetes or vitamin deficiency, or the local effects of chronic tobacco or alcohol use. The oral mucosa tends to heal faster and with less scar formation compared to the skin. The underlying mechanism remains unknown, but research suggests that extracellular vesicles might be involved.
Epulis fissuratum is a benign hyperplasia of fibrous connective tissue which develops as a reactive lesion to chronic mechanical irritation produced by the flange of a poorly fitting denture. More simply, epulis fissuratum is where excess folds of firm tissue form inside the mouth, as a result of rubbing on the edge of dentures that do not fit well. It is a harmless condition and does not represent oral cancer. Treatment is by simple surgical removal of the lesion, and also by adjustment of the denture or provision of a new denture.
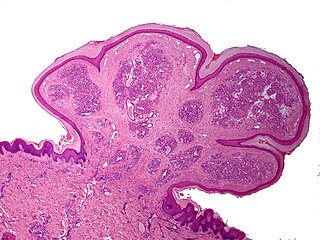
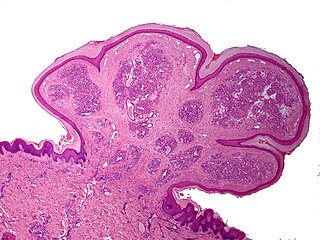
Inflammatory papillary hyperplasia (IPH) is a benign lesion of the oral mucosa which is characterized by the growth of one or more nodular lesions, measuring about 2mm or less. The lesion almost exclusively involves the hard palate, and in rare instances, it also has been seen on the mandible. The lesion is mostly asymptomatic and color of the mucosa may vary from pink to red.
A pyogenic granuloma or lobular capillary hemangioma is a vascular tumor that occurs on both mucosa and skin, and appears as an overgrowth of tissue due to irritation, physical trauma, or hormonal factors. It is often found to involve the gums, skin, or nasal septum, and has also been found far from the head, such as in the thigh.
A peripheral ossifying fibroma, also known as ossifying fibrous epulis, is “a gingival nodule which is composed of a cellular fibroblastic connective tissue stroma which is associated with the formation of randomly dispersed foci of mineralised products, which consists of bone, cementum-like tissue, or a dystrophic calcification. The lesion is considered part of an ossifying fibroma, but that is usually considered to be a jaw tumor. Because of its overwhelming incidence on the gingiva, the condition is associated with two other diseases, though not because they occur together. Instead, the three are associated with each other because they appear frequently on gingiva: pyogenic granuloma and peripheral giant cell granuloma. Some researchers believe peripheral ossifying fibromas to be related to pyogenic fibromas and, in some instances, are the result of a pyogenic granuloma which has undergone fibrosis and calcification.

Verrucous carcinoma (VC) is an uncommon variant of squamous cell carcinoma. This form of cancer is often seen in those who chew tobacco or use snuff orally, so much so that it is sometimes referred to as "Snuff dipper's cancer".

Calcifying odontogenic cyst (COC) is a rare developmental lesion that comes from odontogenic epithelium. It is also known as a calcifying cystic odontogenic tumor, which is a proliferation of odontogenic epithelium and scattered nest of ghost cells and calcifications that may form the lining of a cyst, or present as a solid mass.
An ameloblastic fibroma is a fibroma of the ameloblastic tissue, that is, an odontogenic tumor arising from the enamel organ or dental lamina. It may be either truly neoplastic or merely hamartomatous. In neoplastic cases, it may be labeled an ameloblastic fibrosarcoma in accord with the terminological distinction that reserves the word fibroma for benign tumors and assigns the word fibrosarcoma to malignant ones. It is more common in the first and second decades of life, when odontogenesis is ongoing, than in later decades. In 50% of cases an unerupted tooth is involved.
Oral and maxillofacial pathology refers to the diseases of the mouth, jaws and related structures such as salivary glands, temporomandibular joints, facial muscles and perioral skin. The mouth is an important organ with many different functions. It is also prone to a variety of medical and dental disorders.

Angiofibroma (AGF) is a descriptive term for a wide range of benign skin or mucous membrane lesions in which individuals have: 1) benign papules, i.e. pinhead-sized elevations that lack visible evidence of containing fluid; 2) nodules, i.e. small firm lumps usually >0.1 cm in diameter; and/or 3) tumors, i.e. masses often regarded as ~0.8 cm or larger. AGF lesions share common macroscopic and microscopic appearances. Grossly, AGF lesions consist of multiple papules, one or more skin-colored to erythematous, dome-shaped nodules, or usually just a single tumor. Microscopically, they consist of spindle-shaped and stellate-shaped cells centered around dilated and thin-walled blood vessels in a background of coarse bundles of collagen. Angiofibromas have been divided into different types but commonly a specific type was given multiple and very different names in different studies. The following list gives a brief description of the AFG types and their alternate names.
Oral submucous fibrosis (OSF) is a chronic, complex, premalignant condition of the oral cavity, characterized by juxta-epithelial inflammatory reaction and progressive fibrosis of the submucosal tissues. As the disease progresses, the oral mucosa becomes fibrotic to the point that the person is unable to open the mouth. The condition is remotely linked to oral cancers and is associated with the chewing of areca nut and/or its byproducts, commonly practiced in South and South-East Asian countries. The incidence of OSF has also increased in western countries due to changing habits and population migration.
Oral pigmentation is asymptomatic and does not usually cause any alteration to the texture or thickness of the affected area. The colour can be uniform or speckled and can appear solitary or as multiple lesions. Depending on the site, depth, and quantity of pigment, the appearance can vary considerably.
Epulis is any tumor like enlargement situated on the gingival or alveolar mucosa. The word literally means "(growth) on the gingiva", and describes only the location of the mass and has no further implications on the nature of the lesion. There are three types: fibromatous, ossifying and acanthomatous. The related term parulis refers to a mass of inflamed granulation tissue at the opening of a draining sinus on the alveolus over the root of an infected tooth. Another closely related term is gingival enlargement, which tends to be used where the enlargement is more generalized over the whole gingiva rather than a localized mass.

Cavernous hemangioma, also called cavernous angioma, venous malformation, or cavernoma, is a type of venous malformation due to endothelial dysmorphogenesis from a lesion which is present at birth. A cavernoma in the brain is called a cerebral cavernous malformation or CCM. Despite its designation as a hemangioma, a cavernous hemangioma is not a tumor as it does not display endothelial hyperplasia. The abnormal tissue causes a slowing of blood flow through the cavities, or "caverns". The blood vessels do not form the necessary junctions with surrounding cells, and the structural support from the smooth muscle is hindered, causing leakage into the surrounding tissue. It is the leakage of blood, referred to as hemorrhage, that causes a variety of symptoms known to be associated with the condition.
Gardner fibroma (GF) is a benign fibroblastic tumor. GF tumors typically develop in the dermis and adjacent subcutaneous tissue lying just below the dermis. These tumors typically occur on the back, abdomen, and other superficial sites but in rare cases have been diagnoses in internal sites such as the retroperitoneum and around the large blood vessels in the upper thoracic cavity. The World Health Organization, 2020, classified Gardner fibroma as a benign tumor in the category of fibroblastic and myofibroblastic tumors.