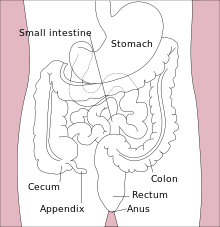
The cecum or caecum is a pouch within the peritoneum that is considered to be the beginning of the large intestine. It is typically located on the right side of the body. The word cecum stems from the Latin caecus meaning blind.

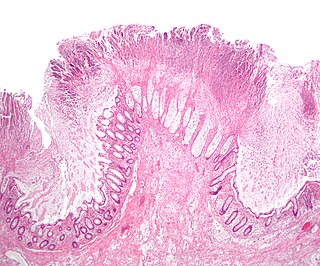
The small intestine or small bowel is an organ in the gastrointestinal tract where most of the absorption of nutrients from food takes place. It lies between the stomach and large intestine, and receives bile and pancreatic juice through the pancreatic duct to aid in digestion. The small intestine is about 5.5 metres long and folds many times to fit in the abdomen. Although it is longer than the large intestine, it is called the small intestine because it is narrower in diameter.
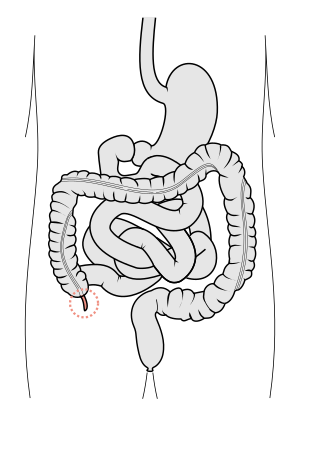
The appendix is a finger-like, blind-ended tube connected to the cecum, from which it develops in the embryo.

Peritonitis is inflammation of the localized or generalized peritoneum, the lining of the inner wall of the abdomen and cover of the abdominal organs. Symptoms may include severe pain, swelling of the abdomen, fever, or weight loss. One part or the entire abdomen may be tender. Complications may include shock and acute respiratory distress syndrome.

Neutropenia is an abnormally low concentration of neutrophils in the blood. Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteria, bacterial fragments and immunoglobulin-bound viruses in the blood. People with neutropenia are more susceptible to bacterial infections and, without prompt medical attention, the condition may become life-threatening.

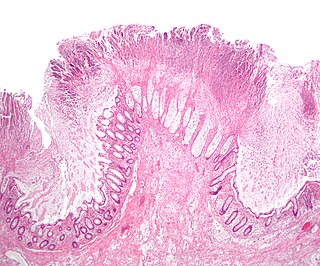
Clostridioides difficile infection, also known as Clostridium difficile infection, is a symptomatic infection due to the spore-forming bacterium Clostridioides difficile. Symptoms include watery diarrhea, fever, nausea, and abdominal pain. It makes up about 20% of cases of antibiotic-associated diarrhea. Antibiotics can contribute to detrimental changes in gut microbiota; specifically, they decrease short-chain fatty acid absorption which results in osmotic, or watery, diarrhea. Complications may include pseudomembranous colitis, toxic megacolon, perforation of the colon, and sepsis.

Enteritis is inflammation of the small intestine. It is most commonly caused by food or drink contaminated with pathogenic microbes, such as Serratia, but may have other causes such as NSAIDs, radiation therapy as well as autoimmune conditions like coeliac disease. Symptoms include abdominal pain, cramping, diarrhoea, dehydration, and fever. Related diseases of the gastrointestinal system involve inflammation of the stomach and large intestine.
Toxic megacolon is an acute form of colonic distension. It is characterized by a very dilated colon (megacolon), accompanied by abdominal distension (bloating), and sometimes fever, abdominal pain, or shock.
Colic in horses is defined as abdominal pain, but it is a clinical symptom rather than a diagnosis. The term colic can encompass all forms of gastrointestinal conditions which cause pain as well as other causes of abdominal pain not involving the gastrointestinal tract. What makes it tricky is that different causes can manifest with similar signs of distress in the animal. Recognizing and understanding these signs is pivotal, as timely action can spell the difference between a brief moment of discomfort and a life-threatening situation. The most common forms of colic are gastrointestinal in nature and are most often related to colonic disturbance. There are a variety of different causes of colic, some of which can prove fatal without surgical intervention. Colic surgery is usually an expensive procedure as it is major abdominal surgery, often with intensive aftercare. Among domesticated horses, colic is the leading cause of premature death. The incidence of colic in the general horse population has been estimated between 4 and 10 percent over the course of the average lifespan. Clinical signs of colic generally require treatment by a veterinarian. The conditions that cause colic can become life-threatening in a short period of time.

Gastrointestinal perforation, also known as gastrointestinal rupture, is a hole in the wall of the gastrointestinal tract. The gastrointestinal tract is composed of hollow digestive organs leading from the mouth to the anus. Symptoms of gastrointestinal perforation commonly include severe abdominal pain, nausea, and vomiting. Complications include a painful inflammation of the inner lining of the abdominal wall and sepsis.

Megacolon is an abnormal dilation of the colon. This leads to hypertrophy of the colon. The dilation is often accompanied by a paralysis of the peristaltic movements of the bowel. In more extreme cases, the feces consolidate into hard masses inside the colon, called fecalomas, which can require surgery to be removed.

Blood in stool looks different depending on how early it enters the digestive tract—and thus how much digestive action it has been exposed to—and how much there is. The term can refer either to melena, with a black appearance, typically originating from upper gastrointestinal bleeding; or to hematochezia, with a red color, typically originating from lower gastrointestinal bleeding. Evaluation of the blood found in stool depends on its characteristics, in terms of color, quantity and other features, which can point to its source, however, more serious conditions can present with a mixed picture, or with the form of bleeding that is found in another section of the tract. The term "blood in stool" is usually only used to describe visible blood, and not fecal occult blood, which is found only after physical examination and chemical laboratory testing.

Rifaximin, is a non-absorbable, broad spectrum antibiotic mainly used to treat travelers' diarrhea. It is based on the rifamycin antibiotics family. Since its approval in Italy in 1987, it has been licensed in over more than 30 countries for the treatment of a variety of gastrointestinal diseases like irritable bowel syndrome, and hepatic encephalopathy. It acts by inhibiting RNA synthesis in susceptible bacteria by binding to the RNA polymerase enzyme. This binding blocks translocation, which stops transcription. It is marketed under the brand name Xifaxan by Salix Pharmaceuticals.
Clostridial necrotizing enteritis (CNE) is a severe and potentially fatal type of food poisoning caused by a β-toxin of Clostridium perfringens, Type C. It occurs in some developing regions, particularly in New Guinea, where it is known as pig-bel. The disease was also documented in Germany following World War II, where it was called Darmbrand (literally "bowel fire," or bowel necrosis). The toxin is normally inactivated by certain proteolytic enzymes and by normal cooking, but when these protections are impeded by diverse factors, and high protein is consumed, the disease can emerge.
Febrile neutropenia is the development of fever, often with other signs of infection, in a patient with neutropenia, an abnormally low number of neutrophil granulocytes in the blood. It is an oncologic emergency, and is the most common serious complication in patients with hematopoietic cancers or receiving chemotherapy for cancer. The term neutropenic sepsis is also applied, although it tends to be reserved for patients who are less well. In 50% of cases, an infection is detectable; bacteremia is present in approximately 20% of all patients with this condition.
Colitis X, equine colitis X or peracute toxemic colitis is a catchall term for various fatal forms of acute or peracute colitis found in horses, but particularly a fulminant colitis where clinical signs include sudden onset of severe diarrhea, abdominal pain, shock, and dehydration. Death is common, with 90–100% mortality, usually in less than 24 hours. The causative factor may be Clostridium difficile, but it also may be caused by other intestinal pathogens. Horses under stress appear to be more susceptible to developing colitis X, and like the condition pseudomembranous colitis in humans, an association with prior antibiotic use also exists. Immediate and aggressive treatment can sometimes save the horse, but even in such cases, 75% mortality is considered a best-case scenario.

Clostridium tertium is an anaerobic, motile, gram-positive bacterium. Although it can be considered an uncommon pathogen in humans, there has been substantial evidence of septic episodes in human beings. C. tertium is easily decolorized in Gram-stained smears and can be mistaken for a Gram-negative organism. However, C.tertium does not grow on selective media for Gram-negative organisms.
Bacteriotherapy is the purposeful use of bacteria or their products in treating an illness. Forms of bacteriotherapy include the use of probiotics, microorganisms that provide health benefits when consumed; fecal matter transplants (FMT) /intestinal microbiota transplant (IMT), the transfer of gut microorganisms from the fecal matter of healthy donors to recipient patients to restore microbiota; or synbiotics which combine prebiotics, indigestible ingredients that promote growth of beneficial microorganisms, and probiotics. Through these methods, the gut microbiota, the community of 300-500 microorganism species that live in the digestive tract of animals aiding in digestion, energy storage, immune function and protection against pathogens, can be recolonized with favorable bacteria, which in turn has therapeutic effects.

Clostridioides difficile is a bacterium known for causing serious diarrheal infections, and may also cause colon cancer. It is known also as C. difficile, or C. diff, and is a Gram-positive species of spore-forming bacteria. Clostridioides spp. are anaerobic, motile bacteria, ubiquitous in nature and especially prevalent in soil. Its vegetative cells are rod-shaped, pleomorphic, and occur in pairs or short chains. Under the microscope, they appear as long, irregular cells with a bulge at their terminal ends. Under Gram staining, C. difficile cells are Gram-positive and show optimum growth on blood agar at human body temperatures in the absence of oxygen. C. difficile is catalase- and superoxide dismutase-negative, and produces up to three types of toxins: enterotoxin A, cytotoxin B and Clostridioides difficile transferase. Under stress conditions, the bacteria produce spores that are able to tolerate extreme conditions that the active bacteria cannot tolerate.
Serum-derived bovine immunoglobulin/protein isolate (SBI) is a medical food product derived from bovine serum obtained from adult cows in the United States. It is sold under the name EnteraGam.