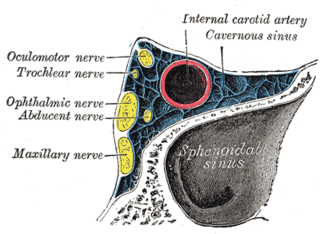
The danger triangle of the face consists of the area from the corners of the mouth to the bridge of the nose, including the nose and maxilla. Due to the special nature of the blood supply to the human nose and surrounding area, it is possible for retrograde infection from the nasal area to spread to the brain, causing cavernous sinus thrombosis, meningitis, or brain abscess.
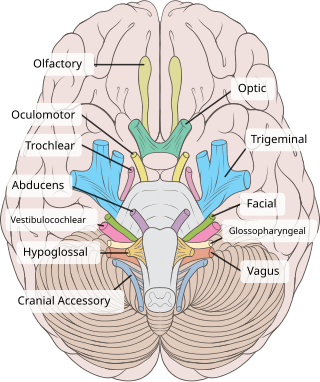
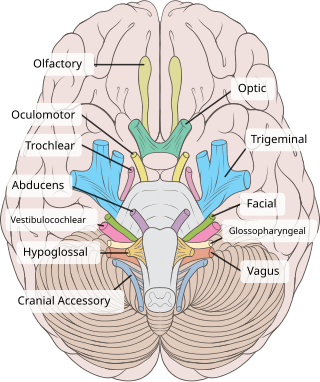
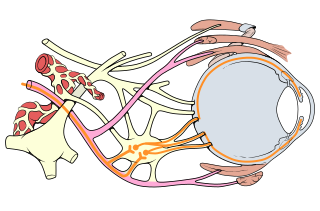
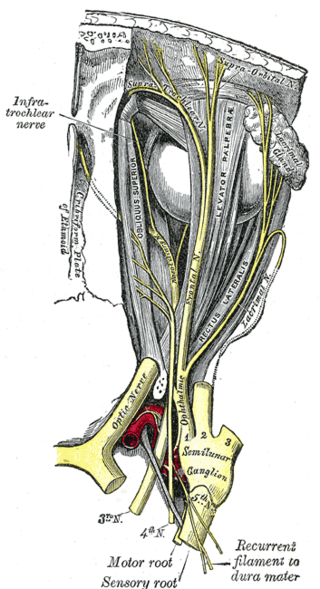
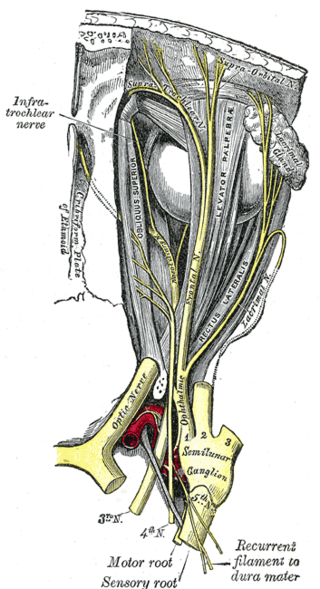
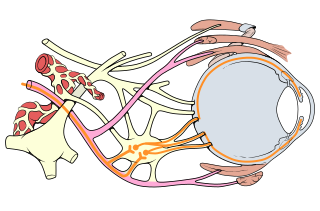
The oculomotor nerve, also known as the third cranial nerve, cranial nerve III, or simply CN III, is a cranial nerve that enters the orbit through the superior orbital fissure and innervates extraocular muscles that enable most movements of the eye and that raise the eyelid. The nerve also contains fibers that innervate the intrinsic eye muscles that enable pupillary constriction and accommodation. The oculomotor nerve is derived from the basal plate of the embryonic midbrain. Cranial nerves IV and VI also participate in control of eye movement.
The supraorbital nerve is one of two terminal branches - the other being the supratrochlear nerve - of the frontal nerve (itself a branch of the ophthalmic nerve (CN V1)). It exits the orbit via the supraorbital foramen/notch before splitting into a medial branch and a lateral branch. It innervates the skin of the forehead, upper eyelid, and the root of the nose.

Horner's syndrome, also known as oculosympathetic paresis, is a combination of symptoms that arises when a group of nerves known as the sympathetic trunk is damaged. The signs and symptoms occur on the same side (ipsilateral) as it is a lesion of the sympathetic trunk. It is characterized by miosis, partial ptosis, apparent anhidrosis, with apparent enophthalmos.
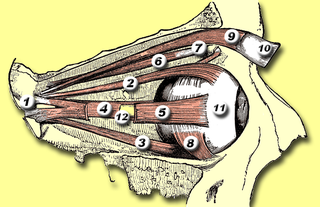
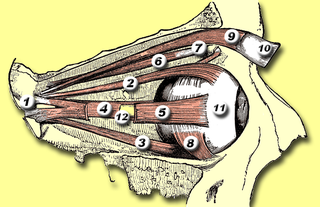
The levator palpebrae superioris is the muscle in the orbit that elevates the upper eyelid.

The extraocular muscles, or extrinsic ocular muscles, are the seven extrinsic muscles of the eye in humans and other animals. Six of the extraocular muscles, the four recti muscles, and the superior and inferior oblique muscles, control movement of the eye. The other muscle, the levator palpebrae superioris, controls eyelid elevation. The actions of the six muscles responsible for eye movement depend on the position of the eye at the time of muscle contraction.
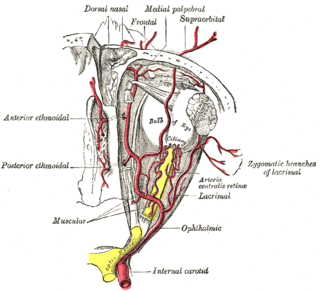
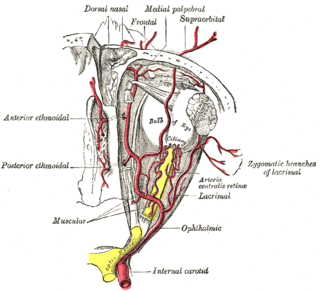
The ophthalmic artery (OA) is an artery of the head. It is the first branch of the internal carotid artery distal to the cavernous sinus. Branches of the ophthalmic artery supply all the structures in the orbit around the eye, as well as some structures in the nose, face, and meninges. Occlusion of the ophthalmic artery or its branches can produce sight-threatening conditions.
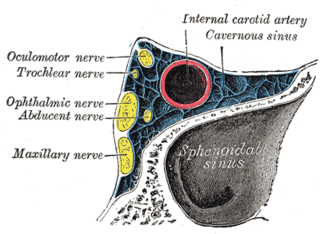
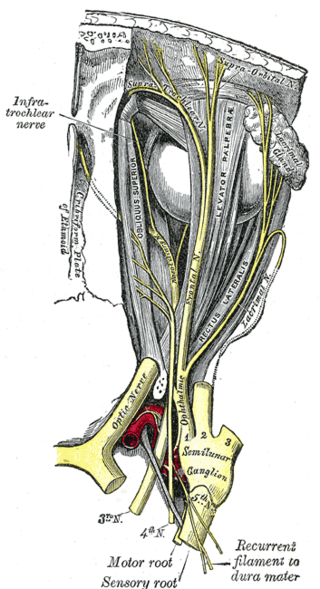
The ophthalmic nerve (CN V1) is a sensory nerve of the head. It is one of three divisions of the trigeminal nerve (CN V), a cranial nerve. It has three major branches which provide sensory innervation to the eye, and the skin of the upper face and anterior scalp, as well as other structures of the head.

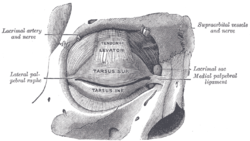
The tarsi or tarsal plates are two comparatively thick, elongated plates of dense connective tissue, about 10 mm (0.39 in) in length for the upper eyelid and 5 mm for the lower eyelid; one is found in each eyelid, and contributes to its form and support. They are located directly above the lid margins. The tarsus has a lower and upper part making up the palpebrae.
The frontal nerve is the largest branch of the ophthalmic nerve (V1), itself a branch of the trigeminal nerve (CN V). It supplies sensation to the skin of the forehead, the mucosa of the frontal sinus, and the skin of the upper eyelid. It may be affected by schwannoma.

The lacrimal nerve is the smallest of the three main branches of the ophthalmic nerve (CN V1) (itself a branch of the trigeminal nerve (CN V)).

The supratrochlear nerve is a branch of the frontal nerve, itself a branch of the ophthalmic nerve (CN V1) from the trigeminal nerve (CN V). It provides sensory innervation to the skin of the forehead and the upper eyelid.
The orbitalis muscle is a vestigial or rudimentary nonstriated muscle that crosses from the infraorbital groove and sphenomaxillary fissure and is intimately united with the periosteum of the orbit. It was described by Heinrich Müller and is often called Müller's muscle. It lies at the back of the orbit and spans the infraorbital fissure. It is a thin layer of smooth muscle that bridges the inferior orbital fissure. It is supplied by sympathetic nerves, and its function is unknown.

Ptosis, also known as blepharoptosis, is a drooping or falling of the upper eyelid. This condition is sometimes called "lazy eye", but that term normally refers to the condition amblyopia. If severe enough and left untreated, the drooping eyelid can cause other conditions, such as amblyopia or astigmatism, so it is especially important to treat the disorder in children before it can interfere with vision development.

Marcus Gunn phenomenon is an autosomal dominant condition with incomplete penetrance, in which nursing infants will have rhythmic upward jerking of their upper eyelid. This condition is characterized as a synkinesis: when two or more muscles that are independently innervated have either simultaneous or coordinated movements.

Weber's syndrome, also known as midbrain stroke syndrome or superior alternating hemiplegia, is a form of stroke that affects the medial portion of the midbrain. It involves oculomotor fascicles in the interpeduncular cisterns and cerebral peduncle so it characterizes the presence of an ipsilateral lower motor neuron type oculomotor nerve palsy and contralateral hemiparesis or hemiplegia.
Oculomotor nerve palsy or oculomotor neuropathy is an eye condition resulting from damage to the third cranial nerve or a branch thereof. As the name suggests, the oculomotor nerve supplies the majority of the muscles controlling eye movements. Damage to this nerve will result in an inability to move the eye normally. The nerve also supplies the upper eyelid muscle and is accompanied by parasympathetic fibers innervating the muscles responsible for pupil constriction. The limitations of eye movement resulting from the condition are generally so severe that patients are often unable to maintain normal eye alignment when gazing straight ahead, leading to strabismus and, as a consequence, double vision (diplopia).

The accessory visual structures are the protecting and supporting structures (adnexa) of the eye, including the eyebrow, eyelids, and lacrimal apparatus. The eyebrows, eyelids, eyelashes, lacrimal gland and drainage apparatus all play a crucial role with regards to globe protection, lubrication, and minimizing the risk of ocular infection. The adnexal structures also help to keep the cornea moist and clean.
Bienfang's test is a clinical test used in the diagnosis of ocular myasthenia gravis. It is used in conjunction with other examination techniques such as Cogan's lid twitch test or enhancement of blepharoptosis from prolonged upward gaze. It is a simple, quick, and non-invasive test for ocular myasthenia gravis that can be performed not only by ophthalmologists or neurologists, but also by other physicians evaluating patients with ptosis, diplopia, or other symptoms of myasthenia gravis.

The ciliary ganglion is a parasympathetic ganglion located just behind the eye in the posterior orbit. Three types of axons enter the ciliary ganglion but only the preganglionic parasympathetic axons synapse there. The entering axons are arranged into three roots of the ciliary ganglion, which join enter the posterior surface of the ganglion.