Serotonin syndrome (SS) is a group of symptoms that may occur with the use of certain serotonergic medications or drugs. The symptoms can range from mild to severe, and are potentially fatal. Symptoms in mild cases include high blood pressure and a fast heart rate; usually without a fever. Symptoms in moderate cases include high body temperature, agitation, increased reflexes, tremor, sweating, dilated pupils, and diarrhea. In severe cases, body temperature can increase to greater than 41.1 °C (106.0 °F). Complications may include seizures and extensive muscle breakdown.
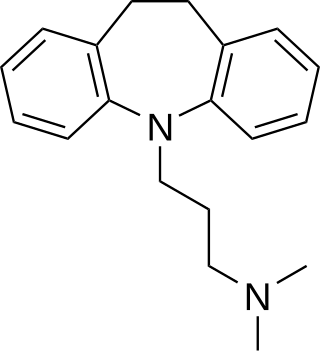
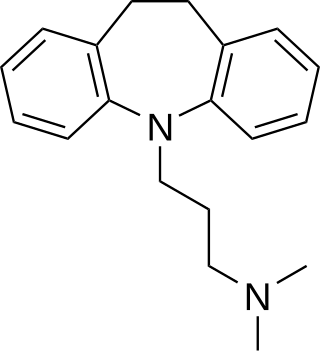
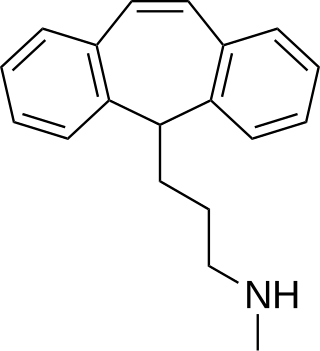
Tricyclic antidepressants (TCAs) are a class of medications that are used primarily as antidepressants. TCAs were discovered in the early 1950s and were marketed later in the decade. They are named after their chemical structure, which contains three rings of atoms. Tetracyclic antidepressants (TeCAs), which contain four rings of atoms, are a closely related group of antidepressant compounds.

Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia. When used for local anaesthesia or in nerve blocks, lidocaine typically begins working within several minutes and lasts for half an hour to three hours. Lidocaine mixtures may also be applied directly to the skin or mucous membranes to numb the area. It is often used mixed with a small amount of adrenaline (epinephrine) to prolong its local effects and to decrease bleeding.

Serotonin–norepinephrine reuptake inhibitors (SNRIs) are a class of antidepressant medications used to treat major depressive disorder (MDD), anxiety disorders, social phobia, chronic neuropathic pain, fibromyalgia syndrome (FMS), and menopausal symptoms. Off-label uses include treatments for attention-deficit hyperactivity disorder (ADHD), obsessive–compulsive disorder (OCD), and migraine prevention. SNRIs are monoamine reuptake inhibitors; specifically, they inhibit the reuptake of serotonin and norepinephrine. These neurotransmitters are thought to play an important role in mood regulation. SNRIs can be contrasted with the selective serotonin reuptake inhibitors (SSRIs) and norepinephrine reuptake inhibitors (NRIs), which act upon single neurotransmitters.
Hypernatremia, also spelled hypernatraemia, is a high concentration of sodium in the blood. Early symptoms may include a strong feeling of thirst, weakness, nausea, and loss of appetite. Severe symptoms include confusion, muscle twitching, and bleeding in or around the brain. Normal serum sodium levels are 135–145 mmol/L. Hypernatremia is generally defined as a serum sodium level of more than 145 mmol/L. Severe symptoms typically only occur when levels are above 160 mmol/L.

Dextropropoxyphene is an analgesic in the opioid category, patented in 1955 and manufactured by Eli Lilly and Company. It is an optical isomer of levopropoxyphene. It is intended to treat mild pain and also has antitussive and local anaesthetic effects. The drug has been taken off the market in Europe and the US due to concerns of fatal overdoses and heart arrhythmias. It is still available in Australia, albeit with restrictions after an application by its manufacturer to review its proposed banning. Its onset of analgesia is said to be 20–30 minutes and peak effects are seen about 1.5–2.0 hours after oral administration.

Clomipramine, sold under the brand name Anafranil among others, is a tricyclic antidepressant (TCA). It is used in the treatment of various conditions, most-notably obsessive–compulsive disorder but also many other disorders, including panic disorder, major depressive disorder, trichotilomania, body dysmorphic disorder and chronic pain. It has also been notably used to treat premature ejaculation and the cataplexy associated with narcolepsy.

Nortriptyline, sold under the brand name Pamelor, among others, is a medication used to treat depression. This medicine is also sometimes used for neuropathic pain, attention deficit hyperactivity disorder (ADHD), smoking cessation and anxiety. As with many antidepressants, its use for young people with depression and other psychiatric disorders may be limited due to increased suicidality in the 18–24 population initiating treatment. Nortriptyline is a less preferred treatment for ADHD and stopping smoking. It is taken by mouth.

Doxepin is a medication belonging to the tricyclic antidepressant (TCA) class of drugs used to treat major depressive disorder, anxiety disorders, chronic hives, and insomnia. For hives it is a less preferred alternative to antihistamines. It has a mild to moderate benefit for sleeping problems. It is used as a cream for itchiness due to atopic dermatitis or lichen simplex chronicus.

Trimipramine, sold under the brand name Surmontil among others, is a tricyclic antidepressant (TCA) which is used to treat depression. It has also been used for its sedative, anxiolytic, and weak antipsychotic effects in the treatment of insomnia, anxiety disorders, and psychosis, respectively. The drug is described as an atypical or "second-generation" TCA because, unlike other TCAs, it seems to be a fairly weak monoamine reuptake inhibitor. Similarly to other TCAs, however, trimipramine does have antihistamine, antiserotonergic, antiadrenergic, antidopaminergic, and anticholinergic activities.

Dosulepin, also known as dothiepin and sold under the brand name Prothiaden among others, is a tricyclic antidepressant (TCA) which is used in the treatment of depression. Dosulepin was once the most frequently prescribed antidepressant in the United Kingdom, but it is no longer widely used due to its relatively high toxicity in overdose without therapeutic advantages over other TCAs. It acts as a serotonin–norepinephrine reuptake inhibitor (SNRI) and also has other activities including antihistamine, antiadrenergic, antiserotonergic, anticholinergic, and sodium channel-blocking effects.

Dibenzepin, sold under the brand name Noveril among others, is a tricyclic antidepressant (TCA) used widely throughout Europe for the treatment of depression. It has similar efficacy and effects relative to other TCAs like imipramine but with fewer side effects.

Lofepramine, sold under the brand names Gamanil, Lomont, and Tymelyt among others, is a tricyclic antidepressant (TCA) which is used to treat depression. The TCAs are so named as they share the common property of having three rings in their chemical structure. Like most TCAs lofepramine is believed to work in relieving depression by increasing concentrations of the neurotransmitters norepinephrine and serotonin in the synapse, by inhibiting their reuptake. It is usually considered a third-generation TCA, as unlike the first- and second-generation TCAs it is relatively safe in overdose and has milder and less frequent side effects.
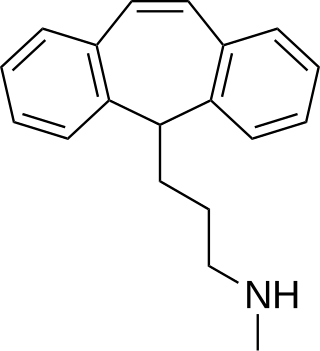
Protriptyline, sold under the brand name Vivactil among others, is a tricyclic antidepressant (TCA), specifically a secondary amine, indicated for the treatment of depression and attention-deficit hyperactivity disorder (ADHD). Uniquely among most of the TCAs, protriptyline tends to be energizing instead of sedating, and is sometimes used for narcolepsy to achieve a wakefulness-promoting effect.

Benzodiazepine overdose describes the ingestion of one of the drugs in the benzodiazepine class in quantities greater than are recommended or generally practiced. The most common symptoms of overdose include central nervous system (CNS) depression, impaired balance, ataxia, and slurred speech. Severe symptoms include coma and respiratory depression. Supportive care is the mainstay of treatment of benzodiazepine overdose. There is an antidote, flumazenil, but its use is controversial.

Salicylate poisoning, also known as aspirin poisoning, is the acute or chronic poisoning with a salicylate such as aspirin. The classic symptoms are ringing in the ears, nausea, abdominal pain, and a fast breathing rate. Early on, these may be subtle, while larger doses may result in fever. Complications can include swelling of the brain or lungs, seizures, low blood sugar, or cardiac arrest.
The Hs and Ts is a mnemonic used to aid in remembering the possible reversible causes of cardiac arrest. A variety of disease processes can lead to a cardiac arrest; however, they usually boil down to one or more of the "Hs and Ts".

Intravenous sodium bicarbonate, also known as sodium hydrogen carbonate, is a medication primarily used to treat severe metabolic acidosis. For this purpose it is generally only used when the pH is less than 7.1 and when the underlying cause is either diarrhea, vomiting, or the kidneys. Other uses include high blood potassium, tricyclic antidepressant overdose, and cocaine toxicity as well as a number of other poisonings. It is given by injection into a vein.

Calcium channel blocker toxicity is the taking of too much of the medications known as calcium channel blockers (CCBs), either by accident or on purpose. This often causes a slow heart rate and low blood pressure. This can progress to the heart stopping altogether. Some CCBs can also cause a fast heart rate as a result of the low blood pressure. Other symptoms may include nausea, vomiting, sleepiness, and shortness of breath. Symptoms usually occur in the first six hours but with some forms of the medication may not start until 24 after hours.

Lithium toxicity, also known as lithium overdose, is the condition of having too much lithium. Symptoms may include a tremor, increased reflexes, trouble walking, kidney problems, and an altered level of consciousness. Some symptoms may last for a year after levels return to normal. Complications may include serotonin syndrome.