 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Eliquis, others |
| Other names | BMS-562247-01 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a613032 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | ~50% |
| Protein binding | ~87% |
| Metabolism | CYP3A4, CYP3A5, CYP1A2 and others |
| Elimination half-life | 9–14 h |
| Excretion | Bile duct (75%), kidney (25%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.167.332 |
| Chemical and physical data | |
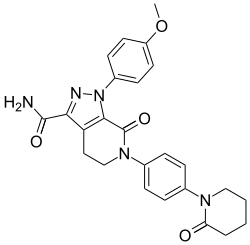
| Formula | C25H25N5O4 |
| Molar mass | 459.506 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Apixaban, sold under the brand name Eliquis, is an anticoagulant medication used to treat and prevent blood clots and to prevent stroke in people with nonvalvular atrial fibrillation through directly inhibiting factor Xa. [8] [9] [10] It is used as an alternative to warfarin to prevent blood clots following hip or knee replacement and in those with a history of prior clots [8] [10] and does not require monitoring by blood tests [8] or dietary restrictions. [11] It is taken by mouth. [8]
Contents
- Medical uses
- Atrial fibrillation
- Side effects
- Bleeding
- Spinal puncture
- Mechanism of action
- History
- Society and culture
- Economics
- References
Common side effects include bleeding and nausea. [8] [9] Other side effects may include bleeding around the spine and allergic reactions. [8] Use is not recommended during pregnancy or breastfeeding. [1] [9] Use appears to be relatively safe in those with mild kidney problems. [9] Compared to warfarin it has fewer interactions with other medications. [12] It is a direct factor Xa inhibitor. [8]
In 2007, Pfizer and Bristol-Myers Squibb began the development of apixaban as an anticoagulant. [13] Apixaban was approved for medical use in the European Union in May 2011, and in the United States in December 2012. [7] [8] [14] It is on the World Health Organization's List of Essential Medicines. [15] In 2023, it was the 28th most commonly prescribed medication in the United States, with more than 19 million prescriptions. [16] [17] It is available as a generic medication, although not in the United States. [10] [18]