 | |
| Clinical data | |
|---|---|
| Other names | vitamin B12, vitamin B12a, hydroxycobalamin |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a605007 |
| Routes of administration | Oral, Intramuscular, intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | Very high (90%) |
| Metabolism | Primarily liver, cobalamins are absorbed in the ileum and stored in the liver. |
| Elimination half-life | ~6 days |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.033.198 |
| Chemical and physical data | |
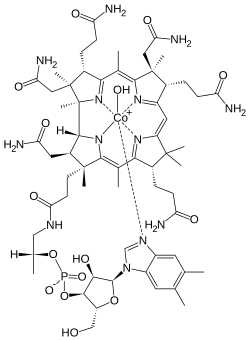
| Formula | C62H89CoN13O15P |
| Molar mass | 1346.377 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Hydroxocobalamin, also known as vitamin B12a and hydroxycobalamin, is a vitamin found in food and used as a dietary supplement. [1] As a supplement it is used to treat vitamin B12 deficiency including pernicious anemia. [1] [2] Other uses include treatment for cyanide poisoning, Leber's optic atrophy, and toxic amblyopia. [3] [4] It is given by injection into a muscle or vein, [2] by pill or sublingually.
Contents
- Medical uses
- Vitamin B12 deficiency
- Cyanide poisoning
- Injectable hydroxocobalamin
- Side effects
- Properties
- Mechanism of action
- See also
- References
Side effects are generally few. [2] They may include diarrhea, feeling sick, hot flushes, itchiness, low blood potassium, allergic reactions, and high blood pressure. [2] Normal doses are considered safe in pregnancy. [5] No overdosage or toxicity has been reported with this drug. [2] Hydroxocobalamin is the natural form of vitamin B12 and a member of the cobalamin family of compounds. [6] [7] It is found in both raw and cooked beef, together with other cobalamins. [8] Hydroxocobalamin, or another form of vitamin B12, are required for the body to make DNA. [7]
Hydroxocobalamin was first isolated in 1949. [9] It is on the World Health Organization's List of Essential Medicines. [10] Hydroxocobalamin is available as a generic medication. [2] Commercially it is made using one of a number of types of bacteria. [11]

