Cetuximab, sold under the brand name Erbitux, is an epidermal growth factor receptor (EGFR) inhibitor medication used for the treatment of metastatic colorectal cancer and head and neck cancer. Cetuximab is a chimeric (mouse/human) monoclonal antibody given by intravenous infusion.

Carcinoembryonic antigen (CEA) describes a set of highly-related glycoproteins involved in cell adhesion. CEA is normally produced in gastrointestinal tissue during fetal development, but the production stops before birth. Consequently, CEA is usually present at very low levels in the blood of healthy adults. However, the serum levels are raised in some types of cancer, which means that it can be used as a tumor marker in clinical tests. Serum levels can also be elevated in heavy smokers.
In biology, chimeric antigen receptors (CARs)—also known as chimeric immunoreceptors, chimeric T cell receptors or artificial T cell receptors—are receptor proteins that have been engineered to give T cells the new ability to target a specific antigen. The receptors are chimeric in that they combine both antigen-binding and T cell activating functions into a single receptor.

Cancer immunotherapy is the stimulation of the immune system to treat cancer, improving on the immune system's natural ability to fight the disease. It is an application of the fundamental research of cancer immunology and a growing subspecialty of oncology.

Targeted therapy or molecularly targeted therapy is one of the major modalities of medical treatment (pharmacotherapy) for cancer, others being hormonal therapy and cytotoxic chemotherapy. As a form of molecular medicine, targeted therapy blocks the growth of cancer cells by interfering with specific targeted molecules needed for carcinogenesis and tumor growth, rather than by simply interfering with all rapidly dividing cells. Because most agents for targeted therapy are biopharmaceuticals, the term biologic therapy is sometimes synonymous with targeted therapy when used in the context of cancer therapy. However, the modalities can be combined; antibody-drug conjugates combine biologic and cytotoxic mechanisms into one targeted therapy.

Radioimmunotherapy (RIT) uses an antibody labeled with a radionuclide to deliver cytotoxic radiation to a target cell. It is a form of unsealed source radiotherapy. In cancer therapy, an antibody with specificity for a tumor-associated antigen is used to deliver a lethal dose of radiation to the tumor cells. The ability for the antibody to specifically bind to a tumor-associated antigen increases the dose delivered to the tumor cells while decreasing the dose to normal tissues. By its nature, RIT requires a tumor cell to express an antigen that is unique to the neoplasm or is not accessible in normal cells.

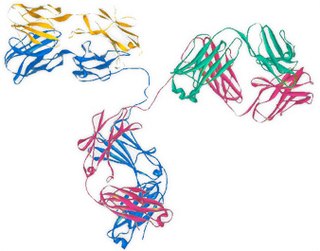
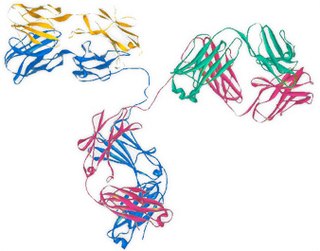
Monoclonal antibody therapy is a form of immunotherapy that uses monoclonal antibodies (mAbs) to bind monospecifically to certain cells or proteins. The objective is that this treatment will stimulate the patient's immune system to attack those cells. Alternatively, in radioimmunotherapy a radioactive dose localizes a target cell line, delivering lethal chemical doses. Antibodies are used to bind to molecules involved in T-cell regulation to remove inhibitory pathways that block T-cell responses. This is known as immune checkpoint therapy.
TroVax is a cancer vaccine that was developed by Oxford BioMedica. No cancer vaccines have been proven to cure cancer or extend life yet, TroVax has been studied in a number of trials for colon cancer.
Abagovomab is a mouse anti-idiotype monoclonal antibody whose variable epitope mirrors a tumour antigen (CA-125) highly expressed in the epithelial ovarian cancer. Abagovomab does not bind directly to CA-125, but it works as a "surrogate" antigen, enabling the immune system to identify and attack tumour cells displaying the CA-125 protein. Through this, it is hoped that the body's immune system may be able to combat any remaining individual tumour cells and thus prevent recurrence of the disease.
Minretumomab (CC49) is a mouse monoclonal antibody that was designed for the treatment of cancers that express the TAG-72 antigen. This includes breast, colon, lung, and pancreatic cancers. Apparently, it never got past Phase I clinical trials for this purpose.

Mesothelin, also known as MSLN, is a protein that in humans is encoded by the MSLN gene.
Tumor-associated glycoprotein 72 (TAG-72) is a glycoprotein found on the surface of many cancer cells, including ovary, breast, colon, lung, and pancreatic cancers. It is a mucin-like molecule with a molar mass of over 1000 kDa.
Siltuximab is a chimeric monoclonal antibody. It binds to interleukin-6. Siltuximab has been investigated for the treatment of neoplastic diseases: metastatic renal cell cancer, prostate cancer, other types of cancer, and for Castleman's disease.
Pelareorep is a proprietary isolate of the unmodified human reovirus being developed as a systemically administered immuno-oncological viral agent for the treatment of solid tumors and hematological malignancies. Pelareorep is an oncolytic virus, which means that it preferentially lyses cancer cells. Pelareorep also promotes an inflamed tumor phenotype through innate and adaptive immune responses. Preliminary clinical trials indicate that it may have anti-cancer effects across a variety of cancer types when administered alone and in combination with other cancer therapies.
Amatuximab is a chimeric monoclonal antibody designed for the treatment of cancer. It was developed by Morphotek, Inc.
Urelumab is a fully human, non‐ligand binding, CD137 agonist immunoglobulin‐γ 4 (IgG4) monoclonal antibody. It was developed utilizing Medarex's UltiMAb(R) technology by Bristol-Myers Squibb for the treatment of cancer and solid tumors. Urelumab promotes anti-tumor immunity, or an immune response against tumor cells, via CD137 activation. The application of Urelumab has been limited due to the fact that it can cause severe liver toxicity.
Ariel Cahill Hollinshead was an American cancer researcher and professor who spent her career at George Washington University. She was a pioneer in discovering tumor antigens and developing them as cancer vaccines.
Globo H (globohexaosylceramide) is a globo-series glycosphingolipid antigen that is present on the outer membrane of some cancer cells. Globo H is not expressed in normal tissue cells, but is expressed in a number of types of cancers, including cancers of the breast, prostate, and pancreas. Globo H's exclusivity for cancer cells makes it a target of interest for cancer therapies.
Passive antibody therapy, also called serum therapy, is a subtype of passive immunotherapy that administers antibodies to target and kill pathogens or cancer cells. It is designed to draw support from foreign antibodies that are donated from a person, extracted from animals, or made in the laboratory to elicit an immune response instead of relying on the innate immune system to fight disease. It has a long history from the 18th century for treating infectious diseases and is now a common cancer treatment. The mechanism of actions include: antagonistic and agonistic reaction, complement-dependent cytotoxicity (CDC), and antibody-dependent cellular cytotoxicity (ADCC).
Lindy Durrant is a British immunologist who is Professor of Cancer Immunotherapy at the University of Nottingham and Chief Scientific Officer and Chief Executive Officer of the UK AIM listed biotech company Scancell Ltd. Durrant's work focusses on harnessing the immune system to treat cancer and infectious disease. Across her career Durrant has developed a panel of monoclonal antibodies which recognise tumour associated glycans, pioneered novel antibody engineering technology to enhance the avidity of monoclonal antibodies as well as developed a number of different cancer vaccine platforms to target cancers such as melanoma, triple negative breast cancer, head and neck cancer amongst others.