Immunotherapy or biological therapy is the treatment of disease by activating or suppressing the immune system. Immunotherapies designed to elicit or amplify an immune response are classified as activation immunotherapies, while immunotherapies that reduce or suppress are classified as suppression immunotherapies. Immunotherapy is under preliminary research for its potential to treat various forms of cancer.

Cancer immunotherapy is the stimulation of the immune system to treat cancer, improving on the immune system's natural ability to fight the disease. It is an application of the fundamental research of cancer immunology and a growing subspecialty of oncology.

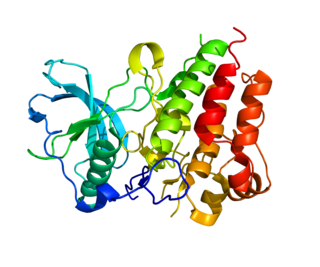
Granulocyte-macrophage colony-stimulating factor (GM-CSF), also known as colony-stimulating factor 2 (CSF2), is a monomeric glycoprotein secreted by macrophages, T cells, mast cells, natural killer cells, endothelial cells and fibroblasts that functions as a cytokine. The pharmaceutical analogs of naturally occurring GM-CSF are called sargramostim and molgramostim.

The colony stimulating factor 1 (CSF1), also known as macrophage colony-stimulating factor (M-CSF), is a secreted cytokine which causes hematopoietic stem cells to differentiate into macrophages or other related cell types. Eukaryotic cells also produce M-CSF in order to combat intercellular viral infection. It is one of the three experimentally described colony-stimulating factors. M-CSF binds to the colony stimulating factor 1 receptor. It may also be involved in development of the placenta.
Chemoimmunotherapy is chemotherapy combined with immunotherapy. Chemotherapy uses different drugs to kill or slow the growth of cancer cells; immunotherapy uses treatments to stimulate or restore the ability of the immune system to fight cancer. A common chemoimmunotherapy regimen is CHOP combined with rituximab (CHOP-R) for B-cell non-Hodgkin lymphomas.
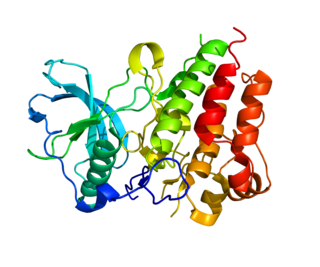
Colony stimulating factor 1 receptor (CSF1R), also known as macrophage colony-stimulating factor receptor (M-CSFR), and CD115, is a cell-surface protein encoded by the human CSF1R gene. CSF1R is a receptor that can be activated by two ligands: colony stimulating factor 1 (CSF-1) and interleukin-34 (IL-34). CSF1R is highly expressed in myeloid cells, and CSF1R signaling is necessary for the survival, proliferation, and differentiation of many myeloid cell types in vivo and in vitro. CSF1R signaling is involved in many diseases and is targeted in therapies for cancer, neurodegeneration, and inflammatory bone diseases.

Triggering receptor expressed on myeloid cells 1 (TREM1) an immunoglobulin (Ig) superfamily transmembrane protein that, in humans, is encoded by the TREM1 gene. TREM1 is constitutively expressed on the surface of peripheral blood monocytes and neutrophils, and upregulated by toll-like receptor (TLR) ligands; activation of TREM1 amplifies immune responses.

Macrophage receptor with collagenous structure (MARCO) is a protein that in humans is encoded by the MARCO gene. MARCO is a class A scavenger receptor that is found on particular subsets of macrophages. Scavenger receptors are pattern recognition receptors (PRRs) found most commonly on immune cells. Their defining feature is that they bind to polyanions and modified forms of a type of cholesterol called low-density lipoprotein (LDL). MARCO is able to bind and phagocytose these ligands and pathogen-associated molecular patterns (PAMPs), leading to the clearance of pathogens and cell signaling events that lead to inflammation. As part of the innate immune system, MARCO clears, or scavenges, pathogens, which leads to inflammatory responses. The scavenger receptor cysteine-rich (SRCR) domain at the end of the extracellular side of MARCO binds ligands to activate the subsequent immune responses. MARCO expression on macrophages has been associated with tumor development and also with Alzheimer's disease, via decreased responses of cells when ligands bind to MARCO.
Tigatuzumab (CS-1008) is a monoclonal antibody for the treatment of cancer. As of October 2009, a clinical trial for the treatment of pancreatic cancer, Phase II trials for colorectal cancer, non-small cell lung cancer, and ovarian cancer have been completed.
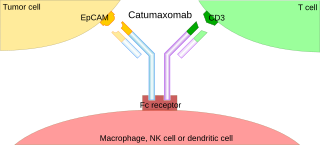
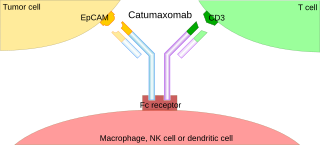
A trifunctional antibody is a monoclonal antibody with binding sites for two different antigens, typically CD3 and a tumor antigen, making it a type of bispecific monoclonal antibody. In addition, its intact Fc-part can bind to an Fc receptor on accessory cells like conventional monospecific antibodies. The net effect is that this type of drug links T cells and monocytes/macrophages, natural killer cells, dendritic cells or other Fc receptor expressing cells to the tumor cells, leading to their destruction.
JX-594 is an oncolytic virus is designed to target and destroy cancer cells. It is also known as Pexa-Vec, INN pexastimogene devacirepvec) and was constructed in Dr. Edmund Lattime's lab at Thomas Jefferson University, tested in clinical trials on melanoma patients, and licensed and further developed by SillaJen.
Urelumab is a fully human, non‐ligand binding, CD137 agonist immunoglobulin‐γ 4 (IgG4) monoclonal antibody. It was developed utilizing Medarex's UltiMAb(R) technology by Bristol-Myers Squibb for the treatment of cancer and solid tumors. Urelumab promotes anti-tumor immunity, or an immune response against tumor cells, via CD137 activation. The application of Urelumab has been limited due to the fact that it can cause severe liver toxicity.
Tumor-associated macrophages (TAMs) are a class of immune cells present in high numbers in the microenvironment of solid tumors. They are heavily involved in cancer-related inflammation. Macrophages are known to originate from bone marrow-derived blood monocytes or yolk sac progenitors, but the exact origin of TAMs in human tumors remains to be elucidated. The composition of monocyte-derived macrophages and tissue-resident macrophages in the tumor microenvironment depends on the tumor type, stage, size, and location, thus it has been proposed that TAM identity and heterogeneity is the outcome of interactions between tumor-derived, tissue-specific, and developmental signals.

The tumor microenvironment (TME) is the environment around a tumor, including the surrounding blood vessels, immune cells, fibroblasts, signaling molecules and the extracellular matrix (ECM). The tumor and the surrounding microenvironment are closely related and interact constantly. Tumors can influence the microenvironment by releasing extracellular signals, promoting tumor angiogenesis and inducing peripheral immune tolerance, while the immune cells in the microenvironment can affect the growth and evolution of cancerous cells.
Myeloid-derived suppressor cells (MDSC) are a heterogeneous group of immune cells from the myeloid lineage.
Dinutuximab and dinutuximab beta are monoclonal antibodies used as a second-line treatment for children with high-risk neuroblastoma. Each antibody is made of both mouse and human components and targets glycolipid GD2, expressed on neuroblastoma cells and on normal cells of neuroectodermal origin, including the central nervous system and peripheral nerves. They differ in that dinutuximab is manufactured using mouse cells, and dinutuximab beta is manufactured using hamster cells. The dosing regime differs, and dinutuximab is given in combination with granulocyte-macrophage colony stimulating factor (GM-CSF), interleukin-2 (IL-2) and 13-cis-retinoic acid (RA), while dinutuximab beta can be given alone.
Lenzilumab is a humanized monoclonal antibody that targets colony stimulating factor 2 (CSF2)/granulocyte-macrophage colony stimulating factor (GM-CSF).

Tenosynovial giant cell tumor (TGCT) is a group of rare, typically non-malignant tumors of the joints. TGCT tumors often develop from the lining of joints.
Naxitamab, sold under the brand name Danyelza, is an anti-cancer medication. It is a monoclonal antibody used in combination with granulocyte-macrophage colony-stimulating factor (GM-CSF) for people one year of age and older with relapsed or refractory high-risk neuroblastoma in the bone or bone marrow demonstrating a partial response, minor response, or stable disease to prior therapy.
Cytokines are polypeptides or glycoproteins that help immune cells communicate to each other to induce proliferation, activation, differentiation, and inflammatory or anti-inflammatory signals in various cell types. Studies utilizing cytokines for antitumor therapies has increased significantly since 2000, and different cytokines provide unique antitumor activities. Cytokines hinder tumor cell development mostly through antiproliferative or proapoptotic pathways but can also interrupt development indirectly by eliciting immune cells to have cytotoxic effects against tumor cells. Even though there are FDA-approved cytokine therapies, there are two main challenges associated with cytokine delivery. The first is that cytokines have a short half-life, so frequent administration of high doses is required for therapeutic effect. The second is that systemic toxicity could occur if the cytokines delivered cause an intense immune response, known as a cytokine storm.