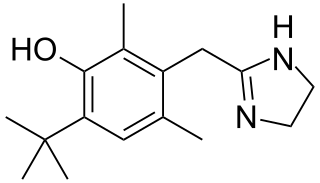
Xylometazoline, also spelled xylomethazoline, is a medication used to reduce symptoms of nasal congestion, allergic rhinitis, and sinusitis. Use is not recommended for more than seven days. Use is also not recommended in those less than three months of age and some say not less than 6 years of age. It is used directly in the nose as a spray or drops.

Allergic rhinitis, of which the seasonal type is called hay fever, is a type of inflammation in the nose that occurs when the immune system overreacts to allergens in the air. Signs and symptoms include a runny or stuffy nose, sneezing, red, itchy, and watery eyes, and swelling around the eyes. The fluid from the nose is usually clear. Symptom onset is often within minutes following allergen exposure, and can affect sleep and the ability to work or study. Some people may develop symptoms only during specific times of the year, often as a result of pollen exposure. Many people with allergic rhinitis also have asthma, allergic conjunctivitis, or atopic dermatitis.
A decongestant, or nasal decongestant, is a type of pharmaceutical drug that is used to relieve nasal congestion in the upper respiratory tract. The active ingredient in most decongestants is either pseudoephedrine or phenylephrine. Intranasal corticosteroids can also be used as decongestants and antihistamines can be used to alleviate runny nose, nasal itch, and sneezing.

Benzalkonium chloride, also known as alkyldimethylbenzylammonium chloride (ADBAC) and by the trade name Zephiran, is a type of cationic surfactant. It is an organic salt classified as a quaternary ammonium compound. ADBACs have three main categories of use: as a biocide, a cationic surfactant, and a phase transfer agent. ADBACs are a mixture of alkylbenzyldimethylammonium chlorides, in which the alkyl group has various even-numbered alkyl chain lengths.

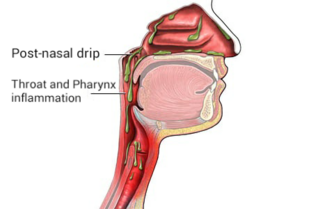
Rhinitis, also known as coryza, is irritation and inflammation of the mucous membrane inside the nose. Common symptoms are a stuffy nose, runny nose, sneezing, and post-nasal drip.
Topical decongestants are decongestants applied directly to the nasal cavity. Their effectiveness by themselves in the common cold appears to have a small benefit in adults.

Ipratropium bromide, sold under the trade name Atrovent among others, is a type of anticholinergic medication which is applied by different routes: inhaler, nebulizer, or nasal spray, for different reasons.

Nasal sprays are used to deliver medications locally in the nasal cavities or systemically. They are used locally for conditions such as nasal congestion and allergic rhinitis. In some situations, the nasal delivery route is preferred for systemic therapy because it provides an agreeable alternative to injection or pills. Substances can be assimilated extremely quickly and directly through the nose. Many pharmaceutical drugs exist as nasal sprays for systemic administration. Other applications include hormone replacement therapy, treatment of Alzheimer's disease and Parkinson's disease. Nasal sprays are seen as a more efficient way of transporting drugs with potential use in crossing the blood–brain barrier.

Phenylephrine is a medication used as a decongestant for uncomplicated nasal congestion, used to dilate the pupil, used to increase blood pressure, and used to relieve hemorrhoids. It can be taken by mouth, as a nasal spray, given by injection into a vein or muscle, or applied to the skin.
Cromoglicic acid (INN)—also referred to as cromolyn (USAN), cromoglycate, or cromoglicate—is traditionally described as a mast cell stabilizer, and is commonly marketed as the sodium salt sodium cromoglicate or cromolyn sodium. This drug prevents the release of inflammatory chemicals such as histamine from mast cells.
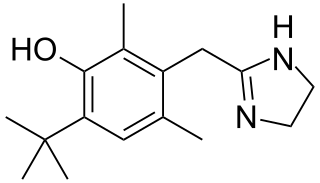
Oxymetazoline, sold under the brand name Afrin among others, is a topical decongestant and vasoconstrictor medication. It is available over-the-counter as a nasal spray to treat nasal congestion and nosebleeds, as eye drops to treat eye redness due to minor irritation, and as a prescription topical cream to treat persistent facial redness due to rosacea in adults. Its effects begin within minutes and last for up to six hours. Intranasal use for longer than three days may cause congestion to recur or worsen, resulting in physical dependence.

Nasal congestion is the partial or complete blockage of nasal passages, leading to impaired nasal breathing, usually due to membranes lining the nose becoming swollen from inflammation of blood vessels.
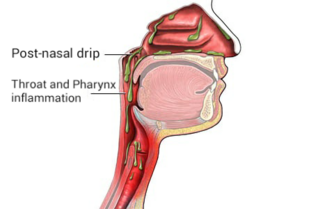
Post-nasal drip (PND), also known as upper airway cough syndrome (UACS), occurs when excessive mucus is produced by the nasal mucosa. The excess mucus accumulates in the back of the nose, and eventually in the throat once it drips down the back of the throat. It can be caused by rhinitis, sinusitis, gastroesophageal reflux disease (GERD), or by a disorder of swallowing. Other causes can be allergy, cold, flu, and side effects from medications.

Naphazoline is a medicine used as a decongestant, and a vasoconstrictor added to eye drops to relieve red eye. It has a rapid action in reducing swelling when applied to mucous membranes. It is a sympathomimetic agent with marked alpha adrenergic activity that acts on alpha-receptors in the arterioles of the conjunctiva to produce constriction, resulting in decreased congestion.

Mometasone, also known as mometasone y 3 s, is a steroid medication used to treat certain skin conditions, hay fever, and asthma. Specifically it is used to prevent rather than treat asthma attacks. It can be applied to the skin, inhaled, or used in the nose. Mometasone furoate, not mometasone, is used in medical products.
Chronic atrophic rhinitis, or simply atrophic rhinitis, is a chronic inflammation of the nose characterised by atrophy of nasal mucosa, including the glands, turbinate bones and the nerve elements supplying the nose. Chronic atrophic rhinitis may be primary and secondary. Special forms of chronic atrophic rhinitis are rhinitis sicca anterior and ozaena. It can also be described as the empty nose syndrome.

Mast cell stabilizers are medications used to prevent or treat certain allergic disorders. They block mast cell degranulation, stabilizing the cell and thereby preventing the release of histamine and related mediators. One suspected pharmacodynamic mechanism is the blocking of IgE-regulated calcium channels. Without intracellular calcium, the histamine vesicles cannot fuse to the cell membrane and degranulate.

Alpha-adrenergic agonists are a class of sympathomimetic agents that selectively stimulates alpha adrenergic receptors. The alpha-adrenergic receptor has two subclasses α1 and α2. Alpha 2 receptors are associated with sympatholytic properties. Alpha-adrenergic agonists have the opposite function of alpha blockers. Alpha adrenoreceptor ligands mimic the action of epinephrine and norepinephrine signaling in the heart, smooth muscle and central nervous system, with norepinephrine being the highest affinity. The activation of α1 stimulates the membrane bound enzyme phospholipase C, and activation of α2 inhibits the enzyme adenylate cyclase. Inactivation of adenylate cyclase in turn leads to the inactivation of the secondary messenger cyclic adenosine monophosphate and induces smooth muscle and blood vessel constriction.
Nonallergic rhinitis is rhinitis—inflammation of the inner part of the nose—not caused by an allergy. Nonallergic rhinitis displays symptoms including chronic sneezing or having a congested, drippy nose, without an identified allergic reaction. Other common terms for nonallergic rhinitis are vasomotor rhinitis and perennial rhinitis. The prevalence of nonallergic rhinitis in otolaryngology is 40%. Allergic rhinitis is more common than nonallergic rhinitis; however, both conditions have similar presentation, manifestation and treatment. Nasal itching and paroxysmal sneezing are usually associated with nonallergic rhinitis rather than allergic rhinitis.
Anti-allergic agents are medications used to treat allergic reactions. Anti-allergic agents have existed since 3000 B.C in countries such as China and Egypt. It was not until 1933 when antihistamines, the first type of anti-allergic agents, were developed. Common allergic diseases include allergic rhinitis, allergic asthma and atopic dermatitis with varying symptoms, including runny nose, watery eyes, itchiness, coughing, and shortness of breath. More than one-third of the world's population is currently being affected by one or more allergic conditions.