Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.

Syringomyelia is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. Often, syringomyelia is used as a generic term before an etiology is determined. This cyst, called a syrinx, can expand and elongate over time, destroying the spinal cord. The damage may result in loss of feeling, paralysis, weakness, and stiffness in the back, shoulders, and extremities. Syringomyelia may also cause a loss of the ability to feel extremes of hot or cold, especially in the hands. It may also lead to a cape-like bilateral loss of pain and temperature sensation along the upper chest and arms. The combination of symptoms varies from one patient to another depending on the location of the syrinx within the spinal cord, as well as its extent.

A brain tumor occurs when abnormal cells form within the brain. There are two main types of tumors: malignant tumors and benign (non-cancerous) tumors. These can be further classified as primary tumors, which start within the brain, and secondary tumors, which most commonly have spread from tumors located outside the brain, known as brain metastasis tumors. All types of brain tumors may produce symptoms that vary depending on the size of the tumor and the part of the brain that is involved. Where symptoms exist, they may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking, with sensations, or unconsciousness.

A cyst is a closed sac, having a distinct envelope and division compared with the nearby tissue. Hence, it is a cluster of cells that have grouped together to form a sac ; however, the distinguishing aspect of a cyst is that the cells forming the "shell" of such a sac are distinctly abnormal when compared with all surrounding cells for that given location. A cyst may contain air, fluids, or semi-solid material. A collection of pus is called an abscess, not a cyst. Once formed, a cyst may resolve on its own. When a cyst fails to resolve, it may need to be removed surgically, but that would depend upon its type and location.

Hydrocephalus is a condition in which an accumulation of cerebrospinal fluid (CSF) occurs within the brain. This typically causes increased pressure inside the skull. Older people may have headaches, double vision, poor balance, urinary incontinence, personality changes, or mental impairment. In babies, it may be seen as a rapid increase in head size. Other symptoms may include vomiting, sleepiness, seizures, and downward pointing of the eyes.

The ventricular system is a set of four interconnected cavities known as cerebral ventricles in the brain. Within each ventricle is a region of choroid plexus which produces the circulating cerebrospinal fluid (CSF). The ventricular system is continuous with the central canal of the spinal cord from the fourth ventricle, allowing for the flow of CSF to circulate.
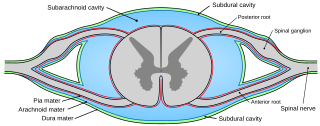
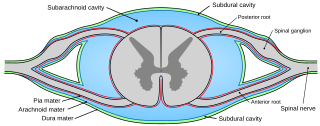
Pia mater, often referred to as simply the pia, is the delicate innermost layer of the meninges, the membranes surrounding the brain and spinal cord. Pia mater is medieval Latin meaning "tender mother". The other two meningeal membranes are the dura mater and the arachnoid mater. Both the pia and arachnoid mater are derivatives of the neural crest while the dura is derived from embryonic mesoderm. The pia mater is a thin fibrous tissue that is permeable to water and small solutes. The pia mater allows blood vessels to pass through and nourish the brain. The perivascular space between blood vessels and pia mater is proposed to be part of a pseudolymphatic system for the brain. When the pia mater becomes irritated and inflamed the result is meningitis.

A dermoid cyst is a teratoma of a cystic nature that contains an array of developmentally mature, solid tissues. It frequently consists of skin, hair follicles, and sweat glands, while other commonly found components include clumps of long hair, pockets of sebum, blood, fat, bone, nail, teeth, eyes, cartilage, and thyroid tissue.

An ependymoma is a tumor that arises from the ependyma, a tissue of the central nervous system. Usually, in pediatric cases the location is intracranial, while in adults it is spinal. The common location of intracranial ependymomas is the fourth ventricle. Rarely, ependymomas can occur in the pelvic cavity.

Astrocytomas are a type of brain tumor. They originate in a particular kind of glial cells, star-shaped brain cells in the cerebrum called astrocytes. This type of tumor does not usually spread outside the brain and spinal cord and it does not usually affect other organs. After glioblastomas, astrocytomas are the second most common glioma and can occur in most parts of the brain and occasionally in the spinal cord.

Pilocytic astrocytoma is a brain tumor that occurs most commonly in children and young adults. They usually arise in the cerebellum, near the brainstem, in the hypothalamic region, or the optic chiasm, but they may occur in any area where astrocytes are present, including the cerebral hemispheres and the spinal cord. These tumors are usually slow growing and benign, corresponding to WHO malignancy grade 1.

Diastematomyelia is a congenital disorder in which a part of the spinal cord is split, usually at the level of the upper lumbar vertebra in the longitudinal (sagittal) direction. Females are affected much more commonly than males. This condition occurs in the presence of an osseous, cartilaginous or fibrous septum in the central portion of the spinal canal which then produces a complete or incomplete sagittal division of the spinal cord into two hemicords. When the split does not reunite distally to the spur, the condition is referred to as diplomyelia, which is true duplication of the spinal cord.

Leptomeningeal cancer is a rare complication of cancer in which the disease spreads from the original tumor site to the meninges surrounding the brain and spinal cord. This leads to an inflammatory response, hence the alternative names neoplastic meningitis (NM), malignant meningitis, or carcinomatous meningitis. The term leptomeningeal describes the thin meninges, the arachnoid and the pia mater, between which the cerebrospinal fluid is located. The disorder was originally reported by Eberth in 1870.

Central nervous system diseases, also known as central nervous system disorders, are a group of neurological disorders that affect the structure or function of the brain or spinal cord, which collectively form the central nervous system (CNS). These disorders may be caused by such things as infection, injury, blood clots, age related degeneration, cancer, autoimmune disfunction, and birth defects. The symptoms vary widely, as do the treatments.

Tarlov cysts, are type II innervated meningeal cysts, cerebrospinal-fluid-filled (CSF) sacs most frequently located in the spinal canal of the sacral region of the spinal cord (S1–S5) and much less often in the cervical, thoracic or lumbar spine. They can be distinguished from other meningeal cysts by their nerve-fiber-filled walls. Tarlov cysts are defined as cysts formed within the nerve-root sheath at the dorsal root ganglion. The etiology of these cysts is not well understood; some current theories explaining this phenomenon have not yet been tested or challenged but include increased pressure in CSF, filling of congenital cysts with one-way valves, inflammation in response to trauma and disease. They are named for American neurosurgeon Isadore Tarlov, who described them in 1938.
Neuro-oncology is the study of brain and spinal cord neoplasms, many of which are very dangerous and life-threatening. Among the malignant brain cancers, gliomas of the brainstem and pons, glioblastoma multiforme, and high-grade astrocytoma/oligodendroglioma are among the worst. In these cases, untreated survival usually amounts to only a few months, and survival with current radiation and chemotherapy treatments may extend that time from around a year to a year and a half, possibly two or more, depending on the patient's condition, immune function, treatments used, and the specific type of malignant brain neoplasm. Surgery may in some cases be curative, but, as a general rule, malignant brain cancers tend to regenerate and emerge from remission easily, especially highly malignant cases. In such cases, the goal is to excise as much of the mass and as much of the tumor margin as possible without endangering vital functions or other important cognitive abilities. The Journal of Neuro-Oncology is the longest continuously published journal in the field and serves as a leading reference to those practicing in the area of neuro-oncology.

Intracranial epidermoid cysts develop in the early embryonic phases. The cysts develop when epithelial cells are confined with cells that form the brain.

A central nervous system primitive neuroectodermal tumor, often abbreviated as PNET, supratentorial PNET, or CNS-PNET, is one of the 3 types of embryonal central nervous system tumors. It is considered an embryonal tumor because it arises from cells partially differentiated or still undifferentiated from birth. Those cells are usually neuroepithelial cells, stem cells destined to turn into glia or neurons. It can occur anywhere within the spinal cord and cerebrum and can have multiple sites of origins, with a high probability of metastasis through cerebrospinal fluid (CSF).
A central nervous system tumor is an abnormal growth of cells from the tissues of the brain or spinal cord. CNS tumor is a generic term encompassing over 120 distinct tumor types. Common symptoms of CNS tumors include vomiting, headache, changes in vision, nausea, and seizures. A CNS tumor can be detected and classified via neurological examination, medical imaging, such as x-ray imaging, magnetic resonance imaging (MRI) or computed tomography (CT), or after analysis of a biopsy.
A lipomyelomeningocele is a type of closed neural tube defect that affects around 3 to 6 babies out of 100,000 births. It is an example of a spinal lipoma, which is a collection of adipose tissue, or fat, that is located at or around the spinal cord. Essentially, it is a tumor of fat located on the spinal cord. A lipomyelomeningocele defect is present at birth and can present with physical defect of the spine and back, and it can also cause various neurological symptoms such as weakness and bladder and bowel incontinence. The general treatment for this spinal defect is surgical detachment of the lipoma from the spine.