Related Research Articles
Amenorrhea or amenorrhoea is the absence of a menstrual period in a female who has reached reproductive age. Physiological states of amenorrhoea are seen, most commonly, during pregnancy and lactation (breastfeeding). Outside the reproductive years, there is absence of menses during childhood and after menopause.
Morning sickness, also called nausea and vomiting of pregnancy (NVP), is a symptom of pregnancy that involves nausea or vomiting. Despite the name, nausea or vomiting can occur at any time during the day. Typically the symptoms occur between the 4th and 16th week of pregnancy. About 10% of women still have symptoms after the 20th week of pregnancy. A severe form of the condition is known as hyperemesis gravidarum and results in weight loss.

Hyperprolactinaemia is a condition characterized by abnormally high levels of prolactin in the blood. In women, normal prolactin levels average to about 13 ng/mL, while in men, they average 5 ng/mL. The upper normal limit of serum prolactin is typically between 15 to 25 ng/mL for both genders. Levels exceeding this range indicate hyperprolactinemia.
Anovulation is when the ovaries do not release an oocyte during a menstrual cycle. Therefore, ovulation does not take place. However, a woman who does not ovulate at each menstrual cycle is not necessarily going through menopause. Chronic anovulation is a common cause of infertility.

Sheehan's syndrome, also known as postpartum pituitary gland necrosis, occurs when the pituitary gland is damaged due to significant blood loss and hypovolemic shock or stroke, originally described during or after childbirth leading to decreased functioning of the pituitary gland (hypopituitarism). Classically, in the milder partial form, the mother is unable to breastfeed her baby, due to failure of the pituitary to secrete the hormone prolactin, and also has no more periods, because FSH and LH are not secreted. Although postmenopausal, the mother with this milder form of Sheehan's syndrome does not experience hot flushes, because the pituitary fails to secrete FSH. The failure to breastfeed and amenorrhea no more periods, were seen as the syndrome, but we now view Sheehan's as the pituitary failing to secrete 1-5 of the 9 hormones that it normally produces (the anterior lobe of the pituitary produces FSH, LH, prolactin, ACTH ,TSH and GH ; the posterior pituitary produces ADH and Oxytocin, i.e. the pituitary is involved in the regulation of many hormones. It is very important to recognise Sheehan' stroke as, the ACTH deficiency Sheehan's in the presence of the stress of a bacterial infection, such as a urine infection, will result in death of the mother from Addisonian crisis. This gland is located on the under-surface of the brain, the shape of a cherry and the size of a chickpea and sits in a pit or depression of the sphenoid bone known as the sella turcica. The pituitary gland works in conjunction with the hypothalamus, and other endocrine organs to modulate numerous bodily functions including growth, metabolism, menstruation, lactation, and even the "fight-or-flight" response. These endocrine organs,, release hormones in very specific pathways, known as hormonal axes. For example, the release of a hormone in the hypothalamus will target the pituitary to trigger the release thyroid stimulating hormone, and the pituitary's released hormone will target the next organ in the pathway i.e. the thyroid to release thyroxin. Hence, damage to the pituitary gland can have downstream effects on any of the aforementioned bodily functions.
Domperidone, sold under the brand name Motilium among others, is a dopamine antagonist medication which is used to treat nausea and vomiting and certain gastrointestinal problems like gastroparesis. It raises the level of prolactin in the human body and is used off label to induce and promote breast milk production. It may be taken by mouth or rectally.
Galactorrhea or lactorrhea is the spontaneous flow of milk from the breast, unassociated with childbirth or nursing.

A prolactinoma is a tumor (adenoma) of the pituitary gland that produces the hormone prolactin. It is the most common type of functioning pituitary tumor. Symptoms of prolactinoma are due to abnormally high levels of prolactin in the blood (hyperprolactinemia), or due to pressure of the tumor on surrounding brain tissue and/or the optic nerves. Based on its size, a prolactinoma may be classified as a microprolactinoma or a macroprolactinoma.
Witch's milk or neonatal milk is milk secreted from the breasts of some newborn human infants of either sex. Production of neonatal milk by infants usually resolves itself and does not require treatment unless it is caused by an underlying condition or medications. It is thought to be caused by the exposure to an elevated level of estrogen to infants during pregnancy or decreased exposure of estrogen to infants after birth. Its production also may be caused by certain medications. The composition of neonatal milk is similar to maternal milk for most of their components except for fats and one type of antibody.

Pregnancy is the time during which one or more offspring develops (gestates) inside a woman's uterus (womb). A multiple pregnancy involves more than one offspring, such as with twins.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.

Sulpiride, sold under the brand name Dogmatil among others, is an atypical antipsychotic medication of the benzamide class which is used mainly in the treatment of psychosis associated with schizophrenia and major depressive disorder, and is sometimes used in low dosage to treat anxiety and mild depression.
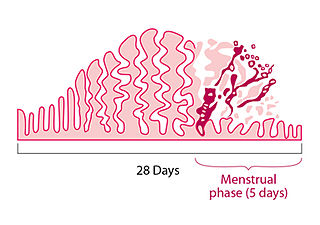
A menstrual disorder is characterized as any abnormal condition with regards to a woman's menstrual cycle. There are many different types of menstrual disorders that vary with signs and symptoms, including pain during menstruation, heavy bleeding, or absence of menstruation. Normal variations can occur in menstrual patterns but generally menstrual disorders can also include periods that come sooner than 21 days apart, more than 3 months apart, or last more than 10 days in duration. Variations of the menstrual cycle are mainly caused by the immaturity of the hypothalamic-pituitary-ovarian (HPO) axis, and early detection and management is required in order to minimize the possibility of complications regarding future reproductive ability.
Primary ovarian insufficiency (POI), also called premature ovarian insufficiency and premature ovarian failure, is the partial or total loss of reproductive and hormonal function of the ovaries before age 40 because of follicular dysfunction or early loss of eggs. POI can be seen as part of a continuum of changes leading to menopause that differ from age-appropriate menopause in the age of onset, degree of symptoms, and sporadic return to normal ovarian function. POI affects approximately 1 in 10,000 women under age 20, 1 in 1,000 women under age 30, and 1 in 100 of those under age 40. A medical triad for the diagnosis is amenorrhea, hypergonadotropism, and hypoestrogenism.

Gallbladder diseases are diseases involving the gallbladder and is closely linked to biliary disease, with the most common cause being gallstones (cholelithiasis).

Postpartum psychosis (PPP), also known as puerperal psychosis or peripartum psychosis, involves the abrupt onset of psychotic symptoms shortly following childbirth, typically within two weeks of delivery but less than 4 weeks postpartum. PPP is a condition currently represented under "Brief Psychotic Disorder" in the Diagnostic and Statistical Manual of Mental Disorders, Volume V (DSM-V). Symptoms may include delusions, hallucinations, disorganized speech, and/or abnormal motor behavior. Other symptoms frequently associated with PPP include confusion, disorganized thought, severe difficulty sleeping, variations of mood disorders, as well as cognitive features such as consciousness that comes and goes or disorientation.
Galactorrhea hyperprolactinemia is increased blood prolactin levels associated with galactorrhea. It may be caused by such things as certain medications, pituitary disorders and thyroid disorders. The condition can occur in males as well as females. Relatively common etiologies include prolactinoma, medication effect, kidney failure, granulomatous diseases of the pituitary gland, and disorders which interfere with the hypothalamic inhibition of prolactin release. Ectopic (non-pituitary) production of prolactin may also occur. Galactorrhea hyperprolactinemia is listed as a “rare disease” by the Office of Rare Diseases of the National Institutes of Health. This means that it affects less than 200,000 people in the United States population.
The term cryptic pregnancy is used by medical professionals to describe a pregnancy that is not recognized by the woman who is pregnant until she is in labor or has given birth. The term is also used online for a special form of false pregnancy (pseudocyesis), or delusion of pregnancy, in which a woman who has no medical verification of pregnancy believes that she is pregnant.
A pre-existing disease in pregnancy is a disease that is not directly caused by the pregnancy, in contrast to various complications of pregnancy, but which may become worse or be a potential risk to the pregnancy. A major component of this risk can result from necessary use of drugs in pregnancy to manage the disease.
Women's reproductive health in the United States refers to the set of physical, mental, and social issues related to the health of women in the United States. It includes the rights of women in the United States to adequate sexual health, available contraception methods, and treatment for sexually transmitted diseases. The prevalence of women's health issues in American culture is inspired by second-wave feminism in the United States. As a result of this movement, women of the United States began to question the largely male-dominated health care system and demanded a right to information on issues regarding their physiology and anatomy. The U.S. government has made significant strides to propose solutions, like creating the Women's Health Initiative through the Office of Research on Women's Health in 1991. However, many issues still exist related to the accessibility of reproductive healthcare as well as the stigma and controversy attached to sexual health, contraception, and sexually transmitted diseases.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Azizi M, Elyasi F (September 2017). "Biopsychosocial view to pseudocyesis: A narrative review". International Journal of Reproductive Biomedicine (Review). 15 (9): 535–542. PMC 5894469 . PMID 29662961.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Tarín JJ, Hermenegildo C, García-Pérez MA, Cano A (May 2013). "Endocrinology and physiology of pseudocyesis". Reproductive Biology and Endocrinology (Review). 11: 39. doi: 10.1186/1477-7827-11-39 . PMC 3674939 . PMID 23672289.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Seeman MV (August 2014). "Pseudocyesis, delusional pregnancy, and psychosis: The birth of a delusion". World Journal of Clinical Cases (Review). 2 (8): 338–44. doi: 10.12998/wjcc.v2.i8.338 . PMC 4133423 . PMID 25133144.
- 1 2 3 Bera SC, Sarkar S (2015). "Delusion of pregnancy: a systematic review of 84 cases in the literature". Indian J Psychol Med. 37 (2): 131–7. doi: 10.4103/0253-7176.155609 . PMC 4418242 . PMID 25969595.
- 1 2 3 4 5 6 7 8 Gogia S, Grieb A, Jang A, Gordon MR, Coverdale J (June 2020). "Medical considerations in delusion of pregnancy: a systematic review". J Psychosom Obstet Gynecol. 43 (1): 51–57. doi:10.1080/0167482X.2020.1779696. PMID 32597281. S2CID 220254853.
- 1 2 Trivedi AN, Singh S (November 1998). "Pseudocyesis and its modern perspective". The Australian & New Zealand Journal of Obstetrics & Gynaecology (Case reports). 38 (4): 466–8. doi:10.1111/j.1479-828X.1998.tb03114.x. PMID 9890236. S2CID 39631778.
- ↑ Ibekwe PC, Achor JU (April 2008). "Psychosocial and cultural aspects of pseudocyesis". Indian Journal of Psychiatry (Case report). 50 (2): 112–6. doi: 10.4103/0019-5545.42398 . PMC 2738334 . PMID 19742215.
- 1 2 3 "Pseudocyesis: what exactly is a false pregnancy?". American Pregnancy Association. March 6, 2019. Retrieved July 30, 2020.
- ↑ Li X, Zhang C, Li Y, Yuan J, Lu Q, Wang Y (2019). "Predictive values of the ratio of beta-human chorionic gonadotropin for failure of salpingostomy in ectopic pregnancy". Int J Clin Exp Pathol. 12 (3): 901–908. PMC 6945191 . PMID 31933899.
- ↑ Ahmad MF, Abu MA, Chew KT, Sheng KL, Zakaria MA (March 2018). "A positive urine pregnancy test (UPT) with adnexal mass; ectopic pregnancy is not the ultimate diagnosis". Horm Mol Biol Clin Investig. 34 (2). doi:10.1515/hmbci-2018-0004. PMID 29558344. S2CID 4039766.
- ↑ Starkman MN, Marshall JC, La Ferla J, Kelch RP (1985). "Pseudocyesis: psychologic and neuroendocrine interrelationships". Psychosomatic Medicine (Case reports). 47 (1): 46–57. doi:10.1097/00006842-198501000-00005. PMID 3975327. S2CID 2029697.
- 1 2 Campos SJ, Link D (June 1, 2016). "Pseudocyesis". The Journal for Nurse Practitioners. 12 (6): 390–394. doi: 10.1016/j.nurpra.2016.03.009 .
- ↑ Mortimer A, Banbery J (April 1988). "Pseudocyesis preceding psychosis". The British Journal of Psychiatry (Case reports). 152 (4): 562–5. doi:10.1192/bjp.152.4.562. PMID 3167413. S2CID 33659629.
- ↑ Babu GN, Desai G, Chandra PS (July 2015). "Antipsychotics in pregnancy and lactation". Indian Journal of Psychiatry (Review). 57 (Suppl 2): S303-7. doi: 10.4103/0019-5545.161497 . PMC 4539875 . PMID 26330648.
- ↑ Thippaiah SM, George V, Birur B, Pandurangi A (March 2018). "A case of concomitant pseudocyesis and Couvade syndrome variant". Psychopharmacology Bulletin (Case report). 48 (3): 29–32. PMC 5875365 . PMID 29713103.
- 1 2 Rutherford RN (April 10, 1941). "Pseudocyesis". New England Journal of Medicine. 224 (15): 639–644. doi:10.1056/NEJM194104102241505. ISSN 0028-4793.
- 1 2 Daley MD (December 1946). "Pseudocyesis". Postgraduate Medical Journal. 22 (254): 395–9. doi:10.1136/pgmj.22.254.395. PMC 2478462 . PMID 20287291.
- ↑ Svoboda, Elizabeth (December 5, 2006). "All the signs of pregnancy except one: a baby". The New York Times . ISSN 0362-4331 . Retrieved February 16, 2020.
- ↑ Radebaugh, John F (Spring 2005). "House calls with John" (PDF). Dartmouth Medicine: 48–63.
- ↑ James, Susan Donaldson (April 10, 2010). "Doctors perform C-Section and find no baby". ABC News. Retrieved February 16, 2020.
- ↑ Dewhurst, John (January 1984). "The alleged miscarriages of Catherine of Aragon and Anne Boleyn". Medical History. 28 (1): 49–56. doi:10.1017/S0025727300035316. PMC 1139382 . PMID 6387336.
- 1 2 Hunter D (1983). "Hysteria, psychoanalysis, and feminism: the case of Anna O". Feminist Studies. 9 (3): 465–88. doi:10.2307/3177609. hdl: 2027/spo.0499697.0009.304 . JSTOR 3177609. PMID 11620548.
- 1 2 Charlier P, Deo S (October 2017). "The Anna O. mystery: Hysteria or neuro-tuberculosis?". J. Neurol. Sci. 381: 19. doi:10.1016/j.jns.2017.08.006. PMID 28991678. S2CID 39296427.