Related Research Articles

Type 2 diabetes (T2D), formerly known as adult-onset diabetes, is a form of diabetes that is characterized by high blood sugar, insulin resistance, and relative lack of insulin. Common symptoms include increased thirst, frequent urination, and unexplained weight loss. Symptoms may also include increased hunger, feeling tired, and sores that do not heal. Often symptoms come on slowly. Long-term complications from high blood sugar include heart disease, strokes, diabetic retinopathy which can result in blindness, kidney failure, and poor blood flow in the limbs which may lead to amputations. The sudden onset of hyperosmolar hyperglycemic state may occur; however, ketoacidosis is uncommon.

Type 1 diabetes (T1D), previously known as juvenile diabetes, is an autoimmune disease that originates when very little or no insulin is produced by the islets of Langerhans in the pancreas. Insulin is a hormone required for the cells to use blood sugar for energy and it helps regulate normal glucose levels in the bloodstream. Before treatment this results in high blood sugar levels in the body. The common symptoms of this elevated blood sugar are frequent urination, increased thirst, increased hunger, weight loss, and other serious complications. Additional symptoms may include blurry vision, tiredness, and slow wound healing. Symptoms typically develop over a short period of time, often a matter of weeks.
Slowly evolving immune-mediated diabetes, or latent autoimmune diabetes in adults (LADA), is a form of diabetes that exhibits clinical features similar to both type 1 diabetes (T1D) and type 2 diabetes (T2D). It is an autoimmune form of diabetes, similar to T1D, but patients with LADA often show insulin resistance, similar to T2D, and share some risk factors for the disease with T2D. Studies have shown that LADA patients have certain types of antibodies against the insulin-producing cells, and that these cells stop producing insulin more slowly than in T1D patients.
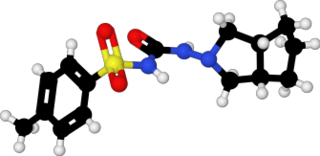
Gliclazide, sold under the brand name Diamicron among others, is a sulfonylurea type of anti-diabetic medication, used to treat type 2 diabetes. It is used when dietary changes, exercise, and weight loss are not enough. It is taken by mouth.
Hepatocyte nuclear factors (HNFs) are a group of phylogenetically unrelated transcription factors that regulate the transcription of a diverse group of genes into proteins. These proteins include blood clotting factors and in addition, enzymes and transporters involved with glucose, cholesterol, and fatty acid transport and metabolism.
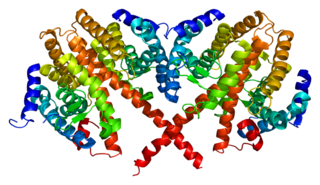
Hepatocyte nuclear factor 4 alpha (HNF4A) also known as NR2A1 is a nuclear receptor that in humans is encoded by the HNF4A gene.

HNF1 homeobox A, also known as HNF1A, is a human gene on chromosome 12. It is ubiquitously expressed in many tissues and cell types. The protein encoded by this gene is a transcription factor that is highly expressed in the liver and is involved in the regulation of the expression of several liver-specific genes. Mutations in the HNF1A gene have been known to cause diabetes. The HNF1A gene also contains one of 27 SNPs associated with increased risk of coronary artery disease.

HNF1 homeobox B, also known as HNF1B or transcription factor 2 (TCF2), is a human gene.

Wolcott–Rallison syndrome,WRS, is a rare, autosomal recessive disorder with infancy-onset diabetes mellitus, multiple epiphyseal dysplasia, osteopenia, mental retardation or developmental delay, and hepatic and renal dysfunction as main clinical findings. Patients with WRS have mutations in the EIF2AK3 gene, which encodes the eukaryotic translation initiation factor 2-alpha kinase 3. Other disease names include multiple epiphyseal dysplasia and early-onset diabetes mellitus. Most patients with this disease do not survive to adulthood. The majority of WRS patients die from fulminant hepatitis during childhood. There are few reported cases for this disease. Of the 54 families worldwide with reported WRS cases, 22.2% of them are from the Kingdom of Saudi Arabia. Of the 23 WRS patients in Saudi Arabia, all but one is the result of consanguineous marriages. Another country where WRS cases have been found is Kosovo. Here, the Albanian population is also known for consanguineous marriages, but there were some cases involving patients from non-consanguineous parents that were carriers for the same mutant allele.

MODY 1 is a form of maturity onset diabetes of the young.
MODY 2 is a form of maturity onset diabetes of the young.
MODY 3 is a form of maturity onset diabetes of the young.
MODY 4 is a form of maturity onset diabetes of the young.

Renal cysts and diabetes syndrome (RCAD), also known as MODY 5, is a form of maturity onset diabetes of the young.
Permanent neonatal diabetes mellitus (PNDM) is a newly identified and potentially treatable form of monogenic diabetes. This type of neonatal diabetes is caused by activating mutations of the KCNJ11 gene, which codes for the Kir6.2 subunit of the beta cell KATP channel. This disease is considered to be a type of maturity onset diabetes of the young (MODY).

Transient neonatal diabetes mellitus (TNDM) is a form of neonatal diabetes presenting at birth that is not permanent. This disease is considered to be a type of maturity onset diabetes of the young (MODY).
Neonatal diabetes mellitus (NDM) is a disease that affects an infant and their body's ability to produce or use insulin. NDM is a monogenic form of diabetes that occurs in the first 6 months of life. Infants do not produce enough insulin, leading to an increase in glucose accumulation. It is a rare disease, occurring in only one in 100,000 to 500,000 live births. NDM can be mistaken for the much more common type 1 diabetes, but type 1 diabetes usually occurs later than the first 6 months of life. There are two types of NDM: permanent neonatal diabetes mellitus (PNDM) is a lifelong condition. Transient neonatal diabetes mellitus (TNDM) is diabetes that disappears during the infant stage but may reappear later in life.
Diabetes usually refers to diabetes mellitus, a group of metabolic diseases in which a person has high blood glucose levels over a prolonged period.
Most cases of type 2 diabetes involved many genes contributing small amount to the overall condition. As of 2011 more than 36 genes have been found that contribute to the risk of type 2 diabetes. All of these genes together still only account for 10% of the total genetic component of the disease.

Diabetes mellitus, commonly known as diabetes, is a group of metabolic disorders characterized by a high blood sugar level over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased appetite. If left untreated, diabetes can cause many health complications. Acute complications can include diabetic ketoacidosis, hyperosmolar hyperglycemic state, or death. Serious long-term complications include cardiovascular disease, stroke, chronic kidney disease, foot ulcers, damage to the nerves, damage to the eyes and cognitive impairment.
References
- ↑ "What is maturity-onset diabetes of the young (MODY)?". National Diabetes Information Clearinghouse (NDIC). National Institute of Diabetes and Digestive and Kidney Diseases, NIH. Archived from the original on 2008-07-04. Retrieved 2008-07-29.
- ↑ Barry J. Goldstein; Dirk Müller-Wieland (2008). Type 2 diabetes: principles and practice. CRC Press. pp. 529–. ISBN 978-0-8493-7957-4 . Retrieved 12 June 2010.
- ↑ Yorifuji, T; Kurokawa, K; Mamada, M; Imai, T; Kawai, M; Nishi, Y; Shishido, S; Hasegawa, Y; Nakahata, T (June 2004). "Neonatal diabetes mellitus and neonatal polycystic, dysplastic kidneys: Phenotypically discordant recurrence of a mutation in the hepatocyte nuclear factor-1beta gene due to germline mosaicism". The Journal of Clinical Endocrinology and Metabolism. 89 (6): 2905–8. doi: 10.1210/jc.2003-031828 . PMID 15181075.
- ↑ Edghill, EL; Bingham, C; Slingerland, AS; Minton, JA; Noordam, C; Ellard, S; Hattersley, AT (December 2006). "Hepatocyte nuclear factor-1 beta mutations cause neonatal diabetes and intrauterine growth retardation: support for a critical role of HNF-1beta in human pancreatic development". Diabetic Medicine. 23 (12): 1301–6. doi:10.1111/j.1464-5491.2006.01999.x. PMID 17116179. S2CID 41113543.
- ↑ This page has previously claimed that MODY is equivalent to type 1 DM; however, the Oxford Handbook of Clinical Medicine states the above.
- ↑ Chennai, India, Dr. V Mohan (2020-07-15). "'Maturity Onset Diabetes of the Young (MODY) | Dr Mohans". Dr Mohan's Diabetes Center in Chennai.
- ↑ Leonid Poretsky (December 2008). Principles of Diabetes Mellitus. Springer. pp. 221–. ISBN 978-0-387-09840-1 . Retrieved 12 June 2010.
- ↑ Steele AM, Shields BM, Wensley KJ, Colclough K, Ellard S, Hattersley AT. (2014). "Prevalence of vascular complications among patients with glucokinase mutations and prolonged, mild hyperglycemia". JAMA. 311 (3): 279–86. doi: 10.1001/jama.2013.283980 . PMID 24430320.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ Dickens LT, Letourneau LR, Sanyoura M, Greeley SAW, Philipson LH, Naylor RN. (2019). "Management and pregnancy outcomes of women with GCK-MODY enrolled in the US Monogenic Diabetes Registry". Acta Diabetologica. 56 (3): 405–411. doi:10.1007/s00592-018-1267-z. PMC 6468988 . PMID 30535721.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ Frayling, TM; Evans, JC; Bulman, MP; Pearson, E (February 2001). "beta-cell genes and diabetes: molecular and clinical characterization of mutations in transcription factors". Diabetes. 50 Suppl (1): S94-100. doi: 10.2337/diabetes.50.2007.S94 . PMID 11272211.
- ↑ Neve B, Fernandez-Zapico ME, Ashkenazi-Katalan V, et al. (March 2005). "Role of transcription factor KLF11 and its diabetes-associated gene variants in pancreatic beta cell function". Proc. Natl. Acad. Sci. U.S.A. 102 (13): 4807–12. doi: 10.1073/pnas.0409177102 . PMC 554843 . PMID 15774581.
- ↑ Online Mendelian Inheritance in Man (OMIM): MATURITY-ONSET DIABETES OF THE YOUNG, TYPE VII; MODY7 - 610508
- ↑ Raeder H, Johansson S, Holm PI, et al. (January 2006). "Mutations in the CEL VNTR cause a syndrome of diabetes and pancreatic exocrine dysfunction". Nat. Genet. 38 (1): 54–62. doi:10.1038/ng1708. PMID 16369531. S2CID 8338877.
- ↑ Online Mendelian Inheritance in Man (OMIM): MATURITY-ONSET DIABETES OF THE YOUNG, TYPE VIII, WITH EXOCRINE DYSFUNCTION; MODY8 - 609812
- ↑ Dhavendra Kumar; D. J. Weatherall (2008). Genomics and clinical medicine. Oxford University Press US. pp. 184–. ISBN 978-0-19-518813-4 . Retrieved 12 June 2010.
- ↑ Urakami T (2019). "Maturity-onset diabetes of the young (MODY): current perspectives on diagnosis and treatment". Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. Diabetes Metabolic Syndrome & Obesity. 12: 1047–1056. doi: 10.2147/DMSO.S179793 . PMC 6625604 . PMID 31360071.
- ↑ MODY (Report). Retrieved Jan 25, 2010.
- ↑ Urbanova J, Rypackova B, Prochazkova Z, Kucera P, Cerna M, Andel M, Heneberg P (2014). "Positivity for islet cell autoantibodies in patients with monogenic diabetes is associated with later diabetes onset and higher HbA1c level". Diabetic Medicine. 31 (4): 466–71. doi:10.1111/dme.12314. PMID 24102923. S2CID 1867195.
- ↑ Maturity Onset Diabetes, SparkPeople, retrieved Jan 21, 2010
- ↑ MODY (Report). Harvard. Retrieved January 23, 2010.
- ↑ Lerario, A. M.; Brito, L. P.; Mariani, B. M.; Fragoso, M. C.; Machado, M. A.; Teixeira, R. (2010). "A missense TCF1 mutation in a patient with MODY-3 and liver adenomatosis". Clinics. 65 (10): 1059–1060. doi:10.1590/S1807-59322010001000024. PMC 2972616 . PMID 21120312.
- ↑ Renal Cysts and Diabetes Syndrome (Report). Retrieved May 19, 2011.
- ↑ "'Maturity Onset Diabetes of the Young (MODY) | Dr Mohans". Dr Mohan's Diabetes Center in Chennai. 15 July 2020.
- ↑ Urbanova, J.; et al. (2015). "Half-Life of Sulfonylureas in HNF1A and HNF4A Human MODY Patients is not Prolonged as Suggested by the Mouse Hnf1a-/- Model". Current Pharmaceutical Design. 21 (39): 5736–5748. doi:10.2174/1381612821666151008124036. PMID 26446475.
- ↑ Galler, Angela; Stange, Thoralf; Müller, Gabriele; Näke, Andrea; Vogel, Christian; Kapellen, Thomas; Bartelt, Heike; Kunath, Hildebrand; Koch, Rainer; Kiess, Wieland; Rothe, Ulrike (2010). "Incidence of Childhood Diabetes in Children Aged Less than 15 Years and Its Clinical and Metabolic Characteristics at the Time of Diagnosis: Data from the Childhood Diabetes Registry of Saxony, Germany". Hormone Research in Paediatrics. 74 (4): 285–91. doi:10.1159/000303141. PMID 20516654. S2CID 1313999.
- ↑ Tattersall RB (1974). "Mild familial diabetes with dominant inheritance". Q J Med. 43 (170): 339–357. PMID 4212169.
- ↑ Tattersall, R (1998). "Maturity-onset diabetes of the young: A clinical history". Diabetic Medicine. 15 (1): 11–4. doi:10.1002/(SICI)1096-9136(199801)15:1<11::AID-DIA561>3.0.CO;2-0. PMID 9472858.
- ↑ American Diabetes, Association (2009). "Diagnosis and Classification of Diabetes Mellitus". Diabetes Care. 32 (Suppl 1): S62–S67. doi:10.2337/dc09-S062. PMC 2613584 . PMID 19118289.