| Pulmonary veno-occlusive disease | |
|---|---|
| Other names | Obstructive disease of the pulmonary veins [1] |
 | |
| Pulmonary veno-occlusive disease-Intimal fibrosis with marked narrowing of lumen of a large pulmonary vein | |
| Specialty | Pulmonology, cardiology |
| Symptoms | Shortness of breath, fatigue [2] |
| Causes | Narrow pulmonary vein, Pulmonary artery hypertension [2] |
| Diagnostic method | Chest x-ray, Chest CT [2] |
| Treatment | Vasodilators can be used [2] |
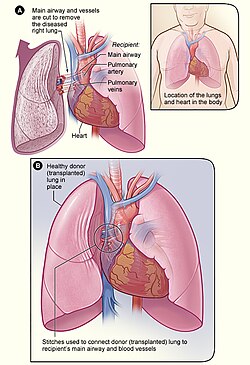
Pulmonary veno-occlusive disease (PVOD) is a rare form of pulmonary hypertension caused by progressive blockage of the small veins in the lungs. [2] The blockage leads to high blood pressures in the arteries of the lungs, which, in turn, leads to heart failure. The disease is progressive and fatal, with median survival of about 2 years from the time of diagnosis to death. [3] The definitive therapy is lung transplantation. [4]