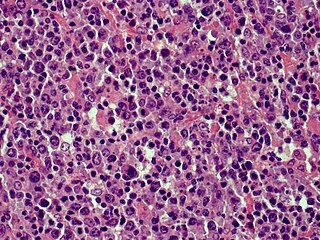
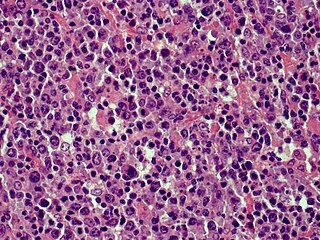
Anaplastic large-cell lymphoma (ALCL) refers to a group of non-Hodgkin lymphomas in which aberrant T cells proliferate uncontrollably. Considered as a single entity, ALCL is the most common type of peripheral lymphoma and represents ~10% of all peripheral lymphomas in children. The incidence of ALCL is estimated to be 0.25 cases per 100,000 people in the United States of America. There are four distinct types of anaplastic large-cell lymphomas that on microscopic examination share certain key histopathological features and tumor marker proteins. However, the four types have very different clinical presentations, gene abnormalities, prognoses, and/or treatments.

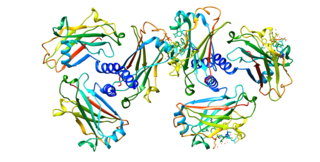
Histone deacetylases (EC 3.5.1.98, HDAC) are a class of enzymes that remove acetyl groups (O=C-CH3) from an ε-N-acetyl lysine amino acid on both histone and non-histone proteins. HDACs allow histones to wrap the DNA more tightly. This is important because DNA is wrapped around histones, and DNA expression is regulated by acetylation and de-acetylation. HDAC's action is opposite to that of histone acetyltransferase. HDAC proteins are now also called lysine deacetylases (KDAC), to describe their function rather than their target, which also includes non-histone proteins. In general, they suppress gene expression.

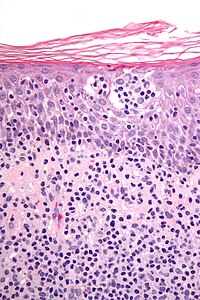
Mycosis fungoides, also known as Alibert-Bazin syndrome or granuloma fungoides, is the most common form of cutaneous T-cell lymphoma. It generally affects the skin, but may progress internally over time. Symptoms include rash, tumors, skin lesions, and itchy skin.
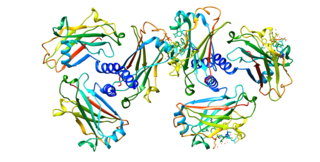
CD30, also known as TNFRSF8, is a cell membrane protein of the tumor necrosis factor receptor family and a tumor marker.

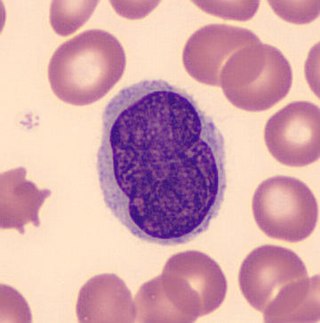
Sézary disease, or Sézary syndrome, is a type of cutaneous T-cell lymphoma that was first described by Albert Sézary. The affected T cells, known as Sézary's cells or Lutzner cells, have pathological quantities of mucopolysaccharides. Sézary disease is sometimes considered a late stage of mycosis fungoides with lymphadenopathy.

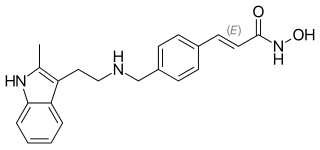
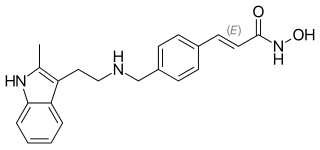
Trichostatin A (TSA) is an organic compound that serves as an antifungal antibiotic and selectively inhibits the class I and II mammalian histone deacetylase (HDAC) families of enzymes, but not class III HDACs. However, there are recent reports of the interactions of this molecule with Sirt 6 protein. TSA inhibits the eukaryotic cell cycle during the beginning of the growth stage. TSA can be used to alter gene expression by interfering with the removal of acetyl groups from histones and therefore altering the ability of DNA transcription factors to access the DNA molecules inside chromatin. It is a member of a larger class of histone deacetylase inhibitors that have a broad spectrum of epigenetic activities. Thus, TSA has some potential as an anti-cancer drug. One suggested mechanism is that TSA promotes the expression of apoptosis-related genes, leading to cancerous cells surviving at lower rates, thus slowing the progression of cancer. Other mechanisms may include the activity of HDIs to induce cell differentiation, thus acting to "mature" some of the de-differentiated cells found in tumors. HDIs have multiple effects on non-histone effector molecules, so the anti-cancer mechanisms are truly not understood at this time.

T-cell lymphoma is a rare form of cancerous lymphoma affecting T-cells. Lymphoma arises mainly from the uncontrolled proliferation of T-cells and can become cancerous.
Vorinostat (rINN), also known as suberoylanilide hydroxamic acid, is a member of a larger class of compounds that inhibit histone deacetylases (HDAC). Histone deacetylase inhibitors (HDI) have a broad spectrum of epigenetic activities.
Panobinostat, sold under the brand name Farydak, is a medication used for the treatment of multiple myeloma. It is a hydroxamic acid and acts as a non-selective histone deacetylase inhibitor.

Pagetoid reticulosis is a cutaneous condition, an uncommon lymphoproliferative disorder, sometimes considered a form of mycosis fungoides.
Primary cutaneous anaplastic large cell lymphoma belongs to the group of cutaneous processes that are CD30+ lymphoproliferative and are characterized by autoregressive, recurrent, single or multifocal ulcerating nodules. Single or localized nodules, papules, or plaques are present in the majority of patients. However, a patient may have more than one lesion in up to 20% of cases.
Cutaneous B-cell lymphomas (CBCL), more recently termed Primary cutaneous B-cell lymphomas and lymphoproliferative disorders (PCBCLPD), are a group of disorders that typically present as skin lesions consisting of proliferating B-cells. B-cells are a type of lymphocyte involved in regulating immune responses. Since its original definition in 1997, CBCL has been considered to have a varying number of subtypes by the European Organisation for Research and Treatment of Cancer, i.e., EORTC, and World Health Organization, i.e., WHO. The latest revised classification of CBCL, which was published by EORTC in 2022, lists the following three main subtypes of CBCL :

Romidepsin, sold under the brand name Istodax, is an anticancer agent used in cutaneous T-cell lymphoma (CTCL) and other peripheral T-cell lymphomas (PTCLs). Romidepsin is a natural product obtained from the bacterium Chromobacterium violaceum, and works by blocking enzymes known as histone deacetylases, thus inducing apoptosis. It is sometimes referred to as depsipeptide, after the class of molecules to which it belongs. Romidepsin is branded and owned by Gloucester Pharmaceuticals, a part of Celgene.
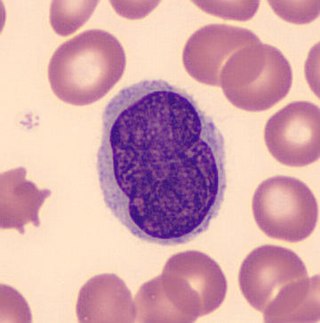
Lutzner cells were discovered by Marvin A. Lutzner, Lucien-Marie Pautrier, and Albert Sézary. These cells are described as the smaller forms of Sézary cells, or Sézary-Lutzner cells, and the two variants are recognised as being morphologically different. Aggregates of these cells in mycosis fungoides are known as a Pautrier's microabscesses. They are a form of T-lymphocytes that have been mutated. This atypical form of T-lymphocytes contains T-cell receptors on the surface and is found in both the dermis and epidermis layers of the skin. Since Lutzner cells are a mutated form of T-lymphocytes, they develop in bone marrow and are transported to the thymus is order to mature. The production and maturation stages occur before the cell has developed a mutation. Lutzner cells can form cutaneous T-cell lymphoma, which is a form of skin cancer.
Brentuximab vedotin, sold under the brand name Adcetris, is an antibody-drug conjugate medication used to treat relapsed or refractory Hodgkin lymphoma (HL) and systemic anaplastic large cell lymphoma (ALCL), a type of T cell non-Hodgkin lymphoma. It selectively targets tumor cells expressing the CD30 antigen, a defining marker of Hodgkin lymphoma and ALCL. The drug is being jointly marketed by Millennium Pharmaceuticals outside the US and by Seagen in the US.
Mogamulizumab, sold under the brand name Poteligeo, is a humanized, afucosylated monoclonal antibody targeting CC chemokine receptor type 4 (CCR4). It is given by injection into a vein.
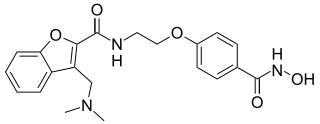
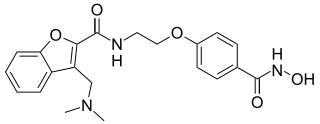
Abexinostat is an experimental drug candidate for cancer treatment. It was developed by Pharmacyclics and licensed to Xynomic. As of 2013, it was in Phase II clinical trials for B-cell lymphoma. Pre-clinical study suggests the potential for treatment of different types of cancer as well.
Mature T-cell lymphoma, also called peripheral T-cell lymphoma, is a group of rare, aggressive lymphomas that develop from mature white blood cells and originate from lymphoid tissues outside of the bone marrow. Mature T-cell lymphoma is under the category of non-Hodgkin lymphoma. Mature T-cell lymphomas account for 10% to 15% of all lymphomas and is more common in Asia than in Europe and America. Its common subtypes include angioimmunoblastic T-cell lymphoma, anaplastic large cell lymphoma and peripheral T-cell lymphoma not otherwise specified. While different subtypes have variable symptoms, common symptoms include enlarged painless lymph nodes, fever, weight loss, rash and night sweats.
Günter Burg is a German dermatologist. Born in Mayen, Germany, he holds German and Swiss citizenship. He has been married to Dr. Doris Burg-Nicklas, a neurologist, since 1968. They have two sons: Andreas and Thomas.
Primary cutaneous acral CD8 positive T cell lymphoproliferative disorder is one type of the lymphoproliferative disorders, subclass cutaneous T-cell lymphoma, in which a slow-growing nodule or papule develops on the ear or, less commonly, other acral sites. CD8 positive T-cells are a subtype of the lymphocytes and acral sites are peripheral parts of the body, i.e., the hands, arms, feet, legs, ears, nose, fingernails, and toenails. In 2007, Petrella et al.,7 reported four patients with tumors composed of CD8+ T-cells and termed the disorder indolent CD8+ lymphoid proliferation of the ear. In 2018, the World Health Organization and European Organisation for Research and Treatment of Cancer provisionally classified this disorder as a lymphoma and termed it primary cutaneous acral CD8 positive T cell lymphoma. In 2022, however, the International Consensus Classification (ICC) group of experts in various medical fields maintained that this disorder was not malignant and therefore termed it primary cutaneous acral CD8 positive T cell lymphoproliferative disorder. In 2024, the World Health Organization (WHO) agreed with this classification and designation. However, histiocyte and CD8 T-cell-rich lymphoproliferations of the skin in individuals with primary immunodeficiency, which had been regarded as a form of CD8+ TLPD, was reclassified as one of the inborn error of immunity-associated lymphoproliferative disorders by the WHO (2022) classification of hematolymphoid tumors. That is, it is now designated as a histiocyte and CD8 T-cell rich lymphoproliferative disorder in patients due to their having an inborn error of immunity. Here, these ICC and WHO classifications are followed, i.e., primary cutaneous acral CD8 positive T cell lymphoma is termed primary cutaneous acral CD8 positive T cell lymphoproliferative disorder and histiocyte and CD8-rich and T-cell-rich lymphoproliferations in associated with a congenital immunodeficiency are not considered to be a form of CD8+ TLPD.