 | |
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | NA |
| Protein binding | 77 to 91% |
| Metabolism | Hepatic |
| Elimination half-life | 1.5 to 2.7 hours |
| Excretion | Renal and biliary |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII |
|
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.035.923 |
| Chemical and physical data | |
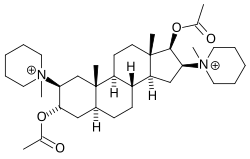
| Formula | C35H60N2O4 |
| Molar mass | 572.875 g·mol−1 |
| |
| | |
Pancuronium (trademarked as Pavulon) is an aminosteroid muscle relaxant with various medical uses. [1] It is used in euthanasia and is used in some states as the second of three drugs administered during lethal injections in the United States.