Anticholinergics are substances that block the action of the acetylcholine (ACh) neurotransmitter at synapses in the central and peripheral nervous system.
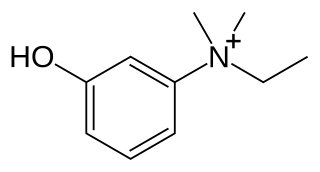
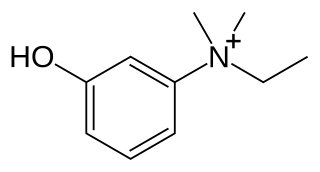
Edrophonium is a readily reversible acetylcholinesterase inhibitor. It prevents breakdown of the neurotransmitter acetylcholine and acts by competitively inhibiting the enzyme acetylcholinesterase, mainly at the neuromuscular junction. It is sold under the trade names Tensilon and Enlon.

A neuromuscular junction is a chemical synapse between a motor neuron and a muscle fiber.
A parasympathomimetic drug, sometimes called a cholinomimetic drug or cholinergic receptor stimulating agent, is a substance that stimulates the parasympathetic nervous system (PSNS). These chemicals are also called cholinergic drugs because acetylcholine (ACh) is the neurotransmitter used by the PSNS. Chemicals in this family can act either directly by stimulating the nicotinic or muscarinic receptors, or indirectly by inhibiting cholinesterase, promoting acetylcholine release, or other mechanisms. Common uses of parasympathomimetics include glaucoma, Sjögren syndrome and underactive bladder.
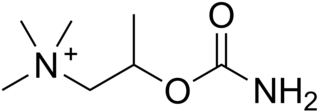
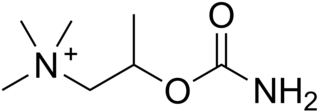
Bethanechol is a parasympathomimetic choline carbamate that selectively stimulates muscarinic receptors without any effect on nicotinic receptors. Unlike acetylcholine, bethanechol is not hydrolyzed by cholinesterase and will therefore have a long duration of action. Bethanechol is sold under the brand names Duvoid (Roberts), Myotonachol (Glenwood), Urecholine, and Urocarb (Hamilton). The name bethanechol refers to its structure as the urethane of beta-methylcholine.
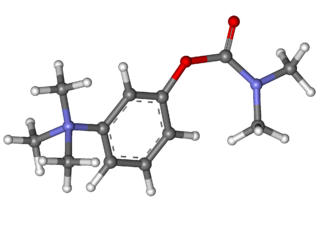
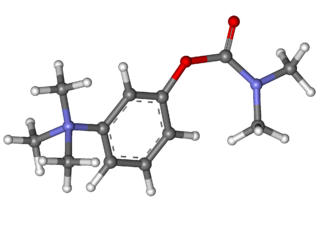
Carbachol, also known as carbamylcholine and sold under the brand name Miostat among others, is a cholinomimetic drug that binds and activates acetylcholine receptors. Thus it is classified as a cholinergic agonist. It is primarily used for various ophthalmic purposes, such as for treating glaucoma, or for use during ophthalmic surgery. It is generally administered as an ophthalmic solution.
Neostigmine, sold under the brand name Bloxiverz, among others, is a medication used to treat myasthenia gravis, Ogilvie syndrome, and urinary retention without the presence of a blockage. It is also used in anaesthesia to end the effects of non-depolarising neuromuscular blocking medication. It is given by injection either into a vein, muscle, or under the skin. After injection effects are generally greatest within 30 minutes and last up to 4 hours.

Physostigmine is a highly toxic parasympathomimetic alkaloid, specifically, a reversible cholinesterase inhibitor. It occurs naturally in the Calabar bean and the fruit of the Manchineel tree.
Orthostatic intolerance (OI) is the development of symptoms when standing upright that are relieved when reclining. There are many types of orthostatic intolerance. OI can be a subcategory of dysautonomia, a disorder of the autonomic nervous system occurring when an individual stands up. Some animal species with orthostatic hypotension have evolved to cope with orthostatic disturbances.

Postural orthostatic tachycardia syndrome (POTS) is a condition characterized by an abnormally large increase in heart rate upon sitting up or standing. POTS is a disorder of the autonomic nervous system that can lead to a variety of symptoms, including lightheadedness, brain fog, blurred vision, weakness, fatigue, headaches, heart palpitations, exercise intolerance, nausea, diminished concentration, tremulousness (shaking), syncope (fainting), coldness or pain in the extremities, numbness or tingling in the extremities, chest pain, and shortness of breath. Other conditions associated with POTS include myalgic encephalomyelitis/chronic fatigue syndrome, migraine headaches, Ehlers–Danlos syndrome, asthma, autoimmune disease, vasovagal syncope, and mast cell activation syndrome. POTS symptoms may be treated with lifestyle changes such as increasing fluid, electrolyte, and salt intake, wearing compression stockings, gentle and slow postural changes, avoiding prolonged bedrest, medication, and physical therapy.

Neuromuscular-blocking drugs, or Neuromuscular blocking agents (NMBAs), block transmission at the neuromuscular junction, causing paralysis of the affected skeletal muscles. This is accomplished via their action on the post-synaptic acetylcholine (Nm) receptors.

Propantheline bromide (INN) is an antimuscarinic medication used for the treatment of excessive sweating (hyperhidrosis), cramps or spasms of the stomach, intestines (gut), or bladder, and involuntary urination (enuresis). It can also be used to control the symptoms of irritable bowel syndrome (IBS) and similar conditions. This medication can also be used for patients who experience intense gastrointestinal symptoms while tapering off of tricyclic antidepressants.
Distigmine is a parasympathomimetic. Distigmine is similar to pyridostigmine and neostigmine but has a longer duration of action. It is available as tablets on prescription only. It is commonly used to treat various conditions, including myasthenia gravis and underactive bladder. Distigmine has a greater risk of causing cholinergic crisis because of accumulation of the drug being more likely than with neostigmine or pyridostigmine and so distigmine is rarely used as a treatment for myasthenia gravis, unlike pyridostigmine and neostigmine.

Acetylcholinesterase (HGNC symbol ACHE; EC 3.1.1.7; systematic name acetylcholine acetylhydrolase), also known as AChE, AChase or acetylhydrolase, is the primary cholinesterase in the body. It is an enzyme that catalyzes the breakdown of acetylcholine and some other choline esters that function as neurotransmitters:

Acetylcholinesterase inhibitors (AChEIs) also often called cholinesterase inhibitors, inhibit the enzyme acetylcholinesterase from breaking down the neurotransmitter acetylcholine into choline and acetate, thereby increasing both the level and duration of action of acetylcholine in the central nervous system, autonomic ganglia and neuromuscular junctions, which are rich in acetylcholine receptors. Acetylcholinesterase inhibitors are one of two types of cholinesterase inhibitors; the other being butyryl-cholinesterase inhibitors. Acetylcholinesterase is the primary member of the cholinesterase enzyme family.

Cholinesterase inhibitors (ChEIs), also known as anti-cholinesterase, are chemicals that prevent the breakdown of the neurotransmitter acetylcholine or butyrylcholine by cholinesterase. This increases the amount of the acetylcholine or butyrylcholine in the synaptic cleft that can bind to muscarinic receptors, nicotinic receptors and others. This group of inhibitors is divided into two subgroups, acetylcholinesterase inhibitors (AChEIs) and butyrylcholinesterase inhibitors (BChEIs).

Underactive bladder syndrome (UAB) describes symptoms of difficulty with bladder emptying, such as hesitancy to start the stream, a poor or intermittent stream, or sensations of incomplete bladder emptying. The physical finding of detrusor activity of insufficient strength or duration to ensure efficient bladder emptying is properly termed "detrusor underactivity" (DU). Historically, UAB and DU have been often used interchangeably, leading to both terminologic and pathophysiologic confusion.
Peripherally selective drugs have their primary mechanism of action outside of the central nervous system (CNS), usually because they are excluded from the CNS by the blood–brain barrier. By being excluded from the CNS, drugs may act on the rest of the body without producing side-effects related to their effects on the brain or spinal cord. For example, most opioids cause sedation when given at a sufficiently high dose, but peripherally selective opioids can act on the rest of the body without entering the brain and are less likely to cause sedation. These peripherally selective opioids can be used as antidiarrheals, for instance loperamide (Imodium).
Autonomic drugs are substances that can either inhibit or enhance the functions of the parasympathetic and sympathetic nervous systems. This type of drug can be used to treat a wide range of diseases an disorders, including glaucoma, asthma, and disorders of the urinary, gastrointestinal and circulatory systems.

Cholinergic blocking drugs are a group of drugs that block the action of acetylcholine (ACh), a neurotransmitter, in synapses of the cholinergic nervous system. They block acetylcholine from binding to cholinergic receptors, namely the nicotinic and muscarinic receptors.