 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | International Drug Names |
| Routes of administration | Oral, Topical, IM |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 25% [1] |
| Elimination half-life | 5-6 hours [1] [2] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.009.107 |
| Chemical and physical data | |
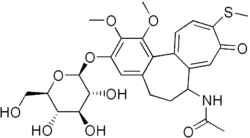
| Formula | C27H33NO10S |
| Molar mass | 563.62 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Thiocolchicoside (Muscoril, Myoril, Neoflax) is a semi-synthetic derivative of colchicine, used as muscle relaxant with anti-inflammatory and analgesic effects. [3] [4] [5] [6] Its mechanism of action is unknown, but it is believed to act via antagonism of nicotinic acetylcholine receptors (nAchRs). However, it also appears to be a competitive antagonist of GABAA and glycine receptors. [7] [8] As such, it has powerful convulsant activity and should not be used in seizure-prone individuals. [9] [10] [11]