| TPP1 | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | TPP1 , CLN2, LPIC, SCAR7, TPP-1, GIG1, Tripeptidyl peptidase I, tripeptidyl peptidase 1 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 607998; MGI: 1336194; HomoloGene: 335; GeneCards: TPP1; OMA:TPP1 - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
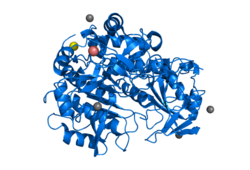
Tripeptidyl-peptidase 1, also known as Lysosomal pepstatin-insensitive protease, is an enzyme that in humans is encoded by the TPP1 gene, also known as CLN2. [5] [6] TPP1 should not be confused with the TPP1 shelterin protein which protects telomeres and is encoded by the ACD gene. [7] Mutations in the TPP1 gene leads to late-infantile neuronal ceroid lipofuscinosis. [8]






