Adenoid cystic carcinoma is a rare type of cancer that can exist in many different body sites. This tumor most often occurs in the salivary glands, but it can also be found in many anatomic sites, including the breast, lacrimal gland, lung, brain, Bartholin gland, trachea, and the paranasal sinuses.

Canalicular adenoma is a benign, epithelial salivary gland neoplasm arranged in interconnecting cords of columnar cells. This is a very rare benign neoplasm, that makes up about 1% of all salivary gland tumors, or about 4% of all benign salivary gland tumors.

Mucoepidermoid carcinoma (MEC) is the most common type of minor salivary gland malignancy in adults. Mucoepidermoid carcinoma can also be found in other organs, such as bronchi, lacrimal sac, and thyroid gland.
Polymorphous low-grade adenocarcinoma (PLGA) is a rare, asymptomatic, slow-growing malignant salivary gland tumor. It is most commonly found in the palate.

Acinic cell carcinoma is a malignant tumor representing 2% of all salivary tumors. 90% of the time found in the parotid gland, 10% intraorally on buccal mucosa or palate. The disease presents as a slow growing mass, associated with pain or tenderness in 50% of the cases. Often appears pseudoencapsulated.

Salivary gland tumours, also known as mucous gland adenomas or neoplasms, are tumours that form in the tissues of salivary glands. The salivary glands are classified as major or minor. The major salivary glands consist of the parotid, submandibular, and sublingual glands. The minor salivary glands consist of 800 to 1000 small mucus-secreting glands located throughout the lining of the oral cavity. Patients with these types of tumours may be asymptomatic.
A mixed tumor is a tumor that derives from multiple tissue types. A biplastic tumor or biphasic tumor has two tissue types.
Juxtaglomerular cell tumor is an extremely rare kidney tumour of the juxtaglomerular cells, with fewer than 100 cases reported in literature. This tumor typically secretes renin, hence the former name of reninoma. It often causes severe hypertension that is difficult to control, in adults and children, although among causes of secondary hypertension it is rare. It develops most commonly in young adults, but can be diagnosed much later in life. It is generally considered benign, but its malignant potential is uncertain.

Eccrine carcinoma is a rare skin condition characterized by a plaque or nodule on the scalp, trunk, or extremities. It originates from the eccrine sweat glands of the skin, accounting for less than 0.01% of diagnosed cutaneous malignancies. Eccrine carcinoma tumors are locally aggressive, with a high rate of recurrence. Lack of reliable immunohistochemical markers and similarity to other common tumors has made identification of eccrine carcinoma difficult.

Metanephric adenoma (MA) is a rare, benign tumour of the kidney, that can have a microscopic appearance similar to a nephroblastoma, or a papillary renal cell carcinoma.

Fetal adenocarcinoma (FA) of the lung is a rare subtype of pulmonary adenocarcinoma that exhibits tissue architecture and cell characteristics that resemble fetal lung tissue upon microscopic examination. It is currently considered a variant of solid adenocarcinoma with mucin production.
Epithelial-myoepithelial carcinoma of the lung is a very rare histologic form of malignant epithelial neoplasm ("carcinoma") arising from lung tissue.

Myoepithelioma of the head and neck, also myoepithelioma, is a salivary gland tumour of the head and neck that is usually benign. When malignant, which is exceedingly rare, they are known as malignant myoepithelioma or Myoepithelial carcinoma, and they account for 1% of the salivary tumors with poor prognosis.

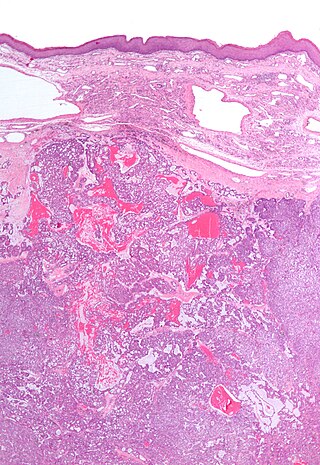
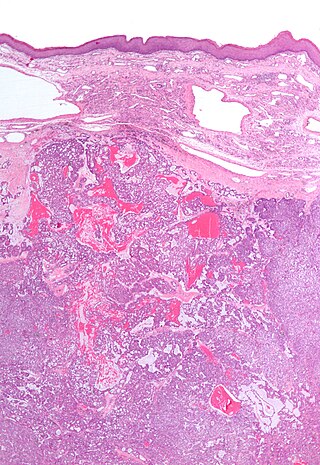
Epithelial-myoepithelial carcinoma (EMCa) is a rare malignant tumour that typically arises in a salivary gland and consists of both an epithelial and myoepithelial component. They are predominantly found in the parotid gland and represent approximately 1% of salivary gland tumours.
A ceruminous adenoma is a benign glandular neoplasm which arises from the ceruminous glands located within the external auditory canal. These glands are found within the outer one third to one half of the external auditory canal, more common along the posterior surface; therefore, the tumor develops within a very specific location.

Ceruminous adenocarcinoma is a malignant neoplasm derived from ceruminous glands of the external auditory canal. This tumor is rare, with several names used in the past. Synonyms have included cylindroma, ceruminoma, ceruminous adenocarcinoma, not otherwise specified (NOS), ceruminous adenoid cystic carcinoma (ACC), and ceruminous mucoepidermoid carcinoma.
Chronic sclerosing sialadenitis is a chronic (long-lasting) inflammatory condition affecting the salivary gland. Relatively rare in occurrence, this condition is benign, but presents as hard, indurated and enlarged masses that are clinically indistinguishable from salivary gland neoplasms or tumors. It is now regarded as a manifestation of IgG4-related disease.

Sclerosing polycystic adenosis is a rare salivary gland tumor first described in 1996 by Dr. Brion Smith. The major salivary glands, specifically the parotid gland and the submandibular gland, are affected most commonly. Patients usually come to clinical attention with a mass or swelling in their salivary glands in the 5th decade of life, with females affected much more commonly than males. Nearly all of the cases reported so far have a benign behavior, although there is a single case that has had an associated malignant transformation.
Ectomesenchymal chondromyxoid tumor (ECT) is a benign intraoral tumor with presumed origin from undifferentiated (ecto)mesenchymal cells. There are some who think it is a myoepithelial tumor type.
Mammary analogue secretory carcinoma (MASC), also termed MASCSG, is a salivary gland neoplasm. It is a secretory carcinoma which shares the microscopic pathologic features with other types of secretory carcinomas including mammary secretory carcinoma, secretory carcinoma of the skin, and salivary gland–type carcinoma of the thyroid. MASCSG was first described by Skálová et al. in 2010. The authors of this report found a chromosome translocation in certain salivary gland tumors, i.e. a (12;15)(p13;q25) fusion gene mutation. The other secretory carcinoma types carry this fusion gene.