Related Research Articles
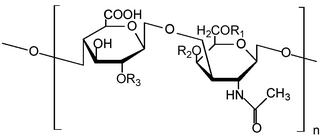
Chondroitin sulfate is a sulfated glycosaminoglycan (GAG) composed of a chain of alternating sugars. It is usually found attached to proteins as part of a proteoglycan. A chondroitin chain can have over 100 individual sugars, each of which can be sulfated in variable positions and quantities. Chondroitin sulfate is an important structural component of cartilage, and provides much of its resistance to compression. Along with glucosamine, chondroitin sulfate has become a widely used dietary supplement for treatment of osteoarthritis, although large clinical trials failed to demonstrate any symptomatic benefit of chondroitin.

Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone which affects 1 in 7 adults in the United States. It is believed to be the fourth leading cause of disability in the world. The most common symptoms are joint pain and stiffness. Usually the symptoms progress slowly over years. Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs, the knee and hip joints, and the joints of the neck and lower back. The symptoms can interfere with work and normal daily activities. Unlike some other types of arthritis, only the joints, not internal organs, are affected.
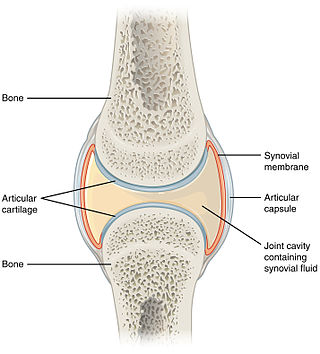
A synovial joint, also known as diarthrosis, joins bones or cartilage with a fibrous joint capsule that is continuous with the periosteum of the joined bones, constitutes the outer boundary of a synovial cavity, and surrounds the bones' articulating surfaces. This joint unites long bones and permits free bone movement and greater mobility. The synovial cavity/joint is filled with synovial fluid. The joint capsule is made up of an outer layer of fibrous membrane, which keeps the bones together structurally, and an inner layer, the synovial membrane, which seals in the synovial fluid.
A chondroitin is a chondrin derivative.

Hyaline cartilage is the glass-like (hyaline) and translucent cartilage found on many joint surfaces. It is also most commonly found in the ribs, nose, larynx, and trachea. Hyaline cartilage is pearl-gray in color, with a firm consistency and has a considerable amount of collagen. It contains no nerves or blood vessels, and its structure is relatively simple.

In medicine, a joint injection is a procedure used in the treatment of inflammatory joint conditions, such as rheumatoid arthritis, psoriatic arthritis, gout, tendinitis, bursitis, Carpal Tunnel Syndrome, and occasionally osteoarthritis. A hypodermic needle is injected into the affected joint where it delivers a dose of any one of many anti-inflammatory agents, the most common of which are corticosteroids. Hyaluronic acid, because of its high viscosity, is sometimes used to replace bursa fluids. The technique may be used to also withdraw excess fluid from the joint.

Pentosan polysulfate, sold under the brand name Elmiron among others, is a medication used for the treatment of interstitial cystitis. It was approved for medical use in the United States in 1996.
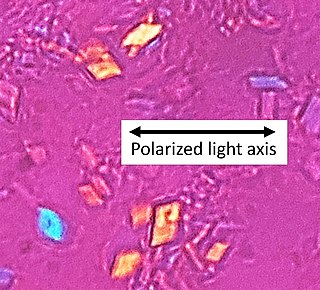
Calcium pyrophosphate dihydrate (CPPD) crystal deposition disease, also known as pseudogout and pyrophosphate arthropathy, is a rheumatologic disease which is thought to be secondary to abnormal accumulation of calcium pyrophosphate dihydrate crystals within joint soft tissues. The knee joint is most commonly affected. The disease is metabolic in origin and its treatment remains symptomatic.

Amtolmetin guacil is a non-steroidal anti-inflammatory drug (NSAID). It is a prodrug of tolmetin sodium.

The natural history of disease is the course a disease takes in individual people from its pathological onset ("inception") until its resolution. The inception of a disease is not a firmly defined concept. The natural history of a disease is sometimes said to start at the moment of exposure to causal agents. Knowledge of the natural history of disease ranks alongside causal understanding in importance for disease prevention and control. Natural history of disease is one of the major elements of descriptive epidemiology.

Fibroblast growth factor 18 (FGF18) is a protein that is encoded by the Fgf18 gene in humans. The protein was first discovered in 1998, when two newly-identified murine genes Fgf17 and Fgf18 were described and confirmed as being closely related by sequence homology to Fgf8. The three proteins were eventually grouped into the FGF8 subfamily, which contains several of the endocrine FGF superfamily members FGF8, FGF17, and FGF18. Subsequent studies identified FGF18's role in promoting chondrogenesis, and an apparent specific activity for the generation of the hyaline cartilage in articular joints.
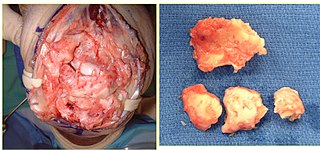
Autologous chondrocyte implantation is a biomedical treatment that repairs damages in articular cartilage. ACI provides pain relief while at the same time slowing down the progression or considerably delaying partial or total joint replacement surgery. The goal of ACI is to allow people suffering from articular cartilage damage to return to their old lifestyle; regaining mobility, going back to work and even practicing sports again.

Licofelone is a dual COX/LOX inhibitor that was studied in clinical trials as a treatment for osteoarthritis and which was under development by Merckle GmbH with partners Alfa Wassermann and Lacer.

Sodium hyaluronate is the sodium salt of hyaluronic acid, a glycosaminoglycan found in various connective tissue of humans.

Arthritis of the knee is typically a particularly debilitating form of arthritis. The knee may become affected by almost any form of arthritis.
Gene therapy is being studied as a treatment for osteoarthritis (OA). Unlike pharmacological treatments which are administered systemically, gene therapy aims to establish sustained, synthesis of gene products and tissue rehabilitation within the joint.
There is a history of clinical research done on glycosaminoglycans, especially glucosamine and chondroitin, for the treatment of arthritis. Since glucosamine is a precursor for glycosaminoglycans, and glycosaminoglycans are major components of cartilage, ingesting glucosamine might nourish joints, and thereby alleviate arthritis symptoms.

Intermittent hydrarthrosis (IH), also known as periodic synoviosis, periodic benign synovitis, or periodic hydrarthritis, is a chronic condition of unknown cause characterized by recurring, temporary episodes of fluid accumulation (effusion) in the knee. While the knee is mainly involved, occasionally other joints such as the elbow or ankle can additionally be affected. Fluid accumulation in the joint can be extensive causing discomfort and impairing movement, although affected joints are not usually very painful. While the condition is chronic, it does not appear to progress to more destructive damage of the joint. It seems to affect slightly more women than men.
Post-traumatic arthritis (PTA) is a form of osteoarthritis following an injury to a joint.
A disease-modifying osteoarthritis drug (DMOAD) is a disease-modifying drug that would inhibit or even reverse the progression of osteoarthritis. Since the main hallmark of osteoarthritis is cartilage loss, a typical DMOAD would prevent the loss of cartilage and potentially regenerate it. Other DMOADs may attempt to help repair adjacent tissues by reducing inflammation. A successful DMOAD would be expected to show an improvement in patient pain and function with an improvement of the health of the joint tissues.
References
- ↑ "Inxight Drugs: Sprifermin". National Center for Advancing Translational Sciences.
- ↑ Gigout A, Guehring H, Froemel D, Meurer A, Ladel C, Reker D, et al. (November 2017). "Sprifermin (rhFGF18) enables proliferation of chondrocytes producing a hyaline cartilage matrix". Osteoarthritis and Cartilage. 25 (11): 1858–1867. doi: 10.1016/j.joca.2017.08.004 . PMID 28823647.
- ↑ "Sprifermin - Merck". Adis Insight. Springer Nature Switzerland AG.
- ↑ Ornitz, David M.; Itoh, Nobuyuki (2015). "The Fibroblast Growth Factor signaling pathway". Wiley Interdisciplinary Reviews. Developmental Biology. 4 (3): 215–266. doi:10.1002/wdev.176. ISSN 1759-7692. PMC 4393358 . PMID 25772309.
- 1 2 3 4 Eckstein F, Hochberg MC, Guehring H, Moreau F, Ona V, Bihlet AR, et al. (August 2021). "Long-term structural and symptomatic effects of intra-articular sprifermin in patients with knee osteoarthritis: 5-year results from the FORWARD study". Annals of the Rheumatic Diseases. 80 (8): 1062–1069. doi:10.1136/annrheumdis-2020-219181. PMC 8292562 . PMID 33962962.
- ↑ Eckstein, Felix; Hochberg, Marc C.; Guehring, Hans; Moreau, Flavie; Ona, Victor; Bihlet, Asger Reinstrup; Byrjalsen, Inger; Andersen, Jeppe Ragnar; Daelken, Benjamin; Guenther, Oliver; Ladel, Christoph; Michaelis, Martin; Conaghan, Philip G. (August 2021). "Long-term structural and symptomatic effects of intra-articular sprifermin in patients with knee osteoarthritis: 5-year results from the FORWARD study". Annals of the Rheumatic Diseases. 80 (8): 1062–1069. doi:10.1136/annrheumdis-2020-219181. ISSN 1468-2060. PMC 8292562 . PMID 33962962.
- ↑ Conaghan, P. G.; Katz, N.; Hunter, D.; Guermazi, A.; Hochberg, M.; Somberg, K.; Clive, J.; Johnson, M.; Goel, N. (2023-06-01). "Pos1348 Effects of Sprifermin on a Novel Outcome of Osteoarthritis Symptom Progression: Post-Hoc Analysis of the Forward Randomized Trial". Annals of the Rheumatic Diseases. 82 (Suppl 1): 1025–1026. doi:10.1136/annrheumdis-2023-eular.2454. ISSN 0003-4967.