Related Research Articles
A growth factor is a naturally occurring substance capable of stimulating cell proliferation, wound healing, and occasionally cellular differentiation. Usually it is a secreted protein or a steroid hormone. Growth factors are important for regulating a variety of cellular processes.

Haematopoiesis is the formation of blood cellular components. All cellular blood components are derived from haematopoietic stem cells. In a healthy adult human, roughly ten billion to a hundred billion new blood cells are produced per day, in order to maintain steady state levels in the peripheral circulation.

A blood cell, also called a hematopoietic cell, hemocyte, or hematocyte, is a cell produced through hematopoiesis and found mainly in the blood. Major types of blood cells include red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes). Together, these three kinds of blood cells add up to a total 45% of the blood tissue by volume, with the remaining 55% of the volume composed of plasma, the liquid component of blood.

Granulocyte colony-stimulating factor, also known as colony-stimulating factor 3, is a glycoprotein that stimulates the bone marrow to produce granulocytes and stem cells and release them into the bloodstream.
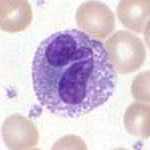
Granulocytes are cells in the innate immune system characterized by the presence of specific granules in their cytoplasm. Such granules distinguish them from the various agranulocytes. All myeloblastic granulocytes are polymorphonuclear. They have varying shapes (morphology) of the nucleus ; and are referred to as polymorphonuclear leukocytes. In common terms, polymorphonuclear granulocyte refers specifically to "neutrophil granulocytes", the most abundant of the granulocytes; the other types have varying morphology. Granulocytes are produced via granulopoiesis in the bone marrow.

Hematopoietic stem cells (HSCs) are the stem cells that give rise to other blood cells. This process is called haematopoiesis. In vertebrates, the very first definitive HSCs arise from the ventral endothelial wall of the embryonic aorta within the (midgestational) aorta-gonad-mesonephros region, through a process known as endothelial-to-hematopoietic transition. In adults, haematopoiesis occurs in the red bone marrow, in the core of most bones. The red bone marrow is derived from the layer of the embryo called the mesoderm.

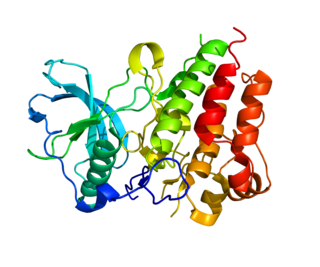
Granulocyte-macrophage colony-stimulating factor (GM-CSF), also known as colony-stimulating factor 2 (CSF2), is a monomeric glycoprotein secreted by macrophages, T cells, mast cells, natural killer cells, endothelial cells and fibroblasts that functions as a cytokine. The pharmaceutical analogs of naturally occurring GM-CSF are called sargramostim and molgramostim.

Interleukin 3 (IL-3) is a protein that in humans is encoded by the IL3 gene localized on chromosome 5q31.1. Sometimes also called colony-stimulating factor, multi-CSF, mast cell growth factor, MULTI-CSF, MCGF; MGC79398, MGC79399: the protein contains 152 amino acids and its molecular weight is 17 kDa. IL-3 is produced as a monomer by activated T cells, monocytes/macrophages and stroma cells. The major function of IL-3 cytokine is to regulate the concentrations of various blood-cell types. It induces proliferation and differentiation in both early pluripotent stem cells and committed progenitors. It also has many more specific effects like the regeneration of platelets and potentially aids in early antibody isotype switching.
Stromal cells, or mesenchymal stromal cells, are differentiating cells found in abundance within bone marrow but can also be seen all around the body. Stromal cells can become connective tissue cells of any organ, for example in the uterine mucosa (endometrium), prostate, bone marrow, lymph node and the ovary. They are cells that support the function of the parenchymal cells of that organ. The most common stromal cells include fibroblasts and pericytes. The term stromal comes from Latin stromat-, "bed covering", and Ancient Greek στρῶμα, strôma, "bed".
Hemopoietic growth factors regulate the differentiation and proliferation of particular progenitor cells. Made available through recombinant DNA technology, they hold tremendous potential for medical uses when a person's natural ability to form blood cells is diminished or defective. Recombinant erythropoietin (EPO) is very effective in treating the diminished red blood cell production that accompanies end-stage kidney disease. Erythropoietin is a sialoglycoprotein hormone produced by peritubular cells of kidney

The colony stimulating factor 1 (CSF1), also known as macrophage colony-stimulating factor (M-CSF), is a secreted cytokine which causes hematopoietic stem cells to differentiate into macrophages or other related cell types. Eukaryotic cells also produce M-CSF in order to combat intercellular viral infection. It is one of the three experimentally described colony-stimulating factors. M-CSF binds to the colony stimulating factor 1 receptor. It may also be involved in development of the placenta.

Granulopoiesis is a part of haematopoiesis, that leads to the production of granulocytes. A granulocyte, also referred to as a polymorphonuclear leukocyte (PMN), is a type of white blood cell that has multi lobed nuclei, usually containing three lobes, and has a significant amount of cytoplasmic granules within the cell. Granulopoiesis takes place in the bone marrow. It leads to the production of three types of mature granulocytes: neutrophils, eosinophils and basophils.

The G-CSF factor stem-loop destabilising element (SLDE) is an RNA element secreted by fibroblasts and endothelial cells in response to the inflammatory mediators interleukin-1 (IL-1) and tumour necrosis factor-alpha and by activated macrophages. The synthesis of G-CSF is regulated both transcriptionally and through control of mRNA stability. In unstimulated cells G-CSF mRNA is unstable but becomes stabilised in response to IL-1 or tumour necrosis factor alpha, and also in the case of monocytes and macrophages, in response to lipopolysaccharide. It is likely that the presence of the SLDE in the G-CSF mRNA contributes to the specificity of regulation of G-CSF mRNA and enhances the rate of shortening of the poly(A) tail.

The granulocyte-macrophage colony-stimulating factor receptor also known as CD116, is a receptor for granulocyte-macrophage colony-stimulating factor, which stimulates the production of white blood cells. In contrast to M-CSF and G-CSF which are lineage specific, GM-CSF and its receptor play a role in earlier stages of development. The receptor is primarily located on neutrophils, eosinophils and monocytes/macrophages, it is also on CD34+ progenitor cells (myeloblasts) and precursors for erythroid and megakaryocytic lineages, but only in the beginning of their development.
Colony stimulating factor 1 receptor (CSF1R), also known as macrophage colony-stimulating factor receptor (M-CSFR), and CD115, is a cell-surface protein encoded by the human CSF1R gene. CSF1R is a receptor that can be activated by two ligands: colony stimulating factor 1 (CSF-1) and interleukin-34 (IL-34). CSF1R is highly expressed in myeloid cells, and CSF1R signaling is necessary for the survival, proliferation, and differentiation of many myeloid cell types in vivo and in vitro. CSF1R signaling is involved in many diseases and is targeted in therapies for cancer, neurodegeneration, and inflammatory bone diseases.

CFU-GM, also known as granulocyte–macrophage progenitor (GMP), is a colony forming unit. It is derived from CFU-GEMM.

CFU-GEMM is a colony forming unit that generates myeloid cells. CFU-GEMM cells are the oligopotential progenitor cells for myeloid cells; they are thus also called common myeloid progenitor cells or myeloid stem cells. "GEMM" stands for granulocyte, erythrocyte, monocyte, megakaryocyte.
CFU-Meg is a colony forming unit. Haematopoiesis in the bone marrow starts off from a haematopoietic stem cell (HSC) and this can differentiate into the myeloid and lymphoid cell lineages. In order to eventually produce a megakaryocyte, the haematopoietic stem cell must generate myeloid cells, so it becomes a common myeloid progenitor, CFU-GEMM. This in turn develops into CFU-Meg, which is the colony forming unit that leads to the production of megakaryocytes.

Reticular dysgenesis (RD) is a rare, inherited autosomal recessive disease that results in immunodeficiency. Individuals with RD have mutations in both copies of the AK2 gene. Mutations in this gene lead to absence of AK2 protein. AK2 protein allows hematopoietic stem cells to differentiate and proliferate. Hematopoietic stem cells give rise to blood cells.
Many human blood cells, such as red blood cells (RBCs), immune cells, and even platelets all originate from the same progenitor cell, the hematopoietic stem cell (HSC). As these cells are short-lived, there needs to be a steady turnover of new blood cells and the maintenance of an HSC pool. This is broadly termed hematopoiesis. This event requires a special environment, termed the hematopoietic stem cell niche, which provides the protection and signals necessary to carry out the differentiation of cells from HSC progenitors. This niche relocates from the yolk sac to eventually rest in the bone marrow of mammals. Many pathological states can arise from disturbances in this niche environment, highlighting its importance in maintaining hematopoiesis.
References
- ↑ Kumar, Vinay; Abbas, Abul K.; Aster, Jon C.; Turner, Jerrold R.; Perkins, James A.; Robbins, Stanley L.; Cotran, Ramzi S., eds. (2021). Robbins & Cotran Pathologic Basis of Disease (10th ed.). Philadelphia, PA: Elsevier. p. 584. ISBN 978-0-323-53113-9.
- Alberts, Bruce; et al. (2002). Molecular Biology of the Cell (4th ed.). New York, NY: Garland Science. ISBN 0-8153-4072-9.