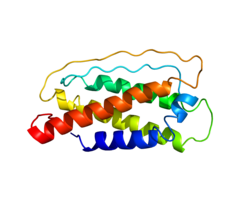
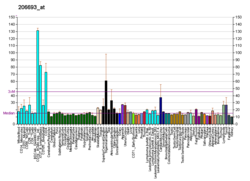
Interleukin 7 (IL-7) is a protein [5] that in humans is encoded by the IL7 gene. [6] [7] [8]
Contents
- Structure
- Function
- Lymphocyte maturation
- IL-7 signaling
- Disease
- Cancer
- Viral Infections
- Clinical application
- Cancer 2
- HIV infection
- Transplantation
- References
- Further reading
IL-7 is a hematopoietic growth factor secreted by stromal cells in the bone marrow and thymus. It is also produced by keratinocytes, [9] follicular dendritic cells, [10] hepatocytes, [11] neurons, and epithelial cells, [12] but is not produced by normal lymphocytes. [13] A study also demonstrated how the autocrine production of the IL-7 cytokine mediated by T-cell acute lymphoblastic leukemia (T-ALL) can be involved in the oncogenic development of T-ALL and offer novel insights into T-ALL spreading. [14]