Immunosuppressive drugs, also known as immunosuppressive agents, immunosuppressants and antirejection medications, are drugs that inhibit or prevent activity of the immune system.
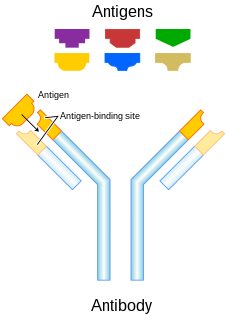
A monoclonal antibody is an antibody made by cloning a unique white blood cell. All subsequent antibodies derived this way trace back to a unique parent cell.
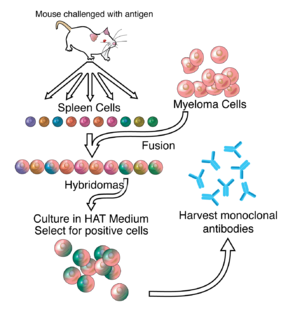
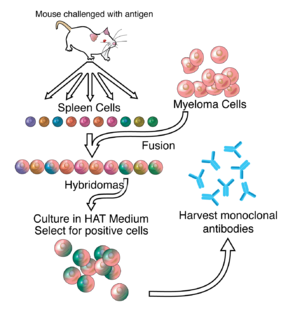
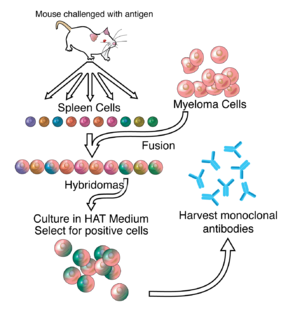
Hybridoma technology is a method for producing large numbers of identical antibodies. This process starts by injecting a mouse with an antigen that provokes an immune response. A type of white blood cell, the B cell, produces antibodies that bind to the injected antigen. These antibody producing B-cells are then harvested from the mouse and, in turn, fused with immortal B cell cancer cells, a myeloma, to produce a hybrid cell line called a hybridoma, which has both the antibody-producing ability of the B-cell and the longevity and reproductivity of the myeloma. The hybridomas can be grown in culture, each culture starting with one viable hybridoma cell, producing cultures each of which consists of genetically identical hybridomas which produce one antibody per culture (monoclonal) rather than mixtures of different antibodies (polyclonal). The myeloma cell line that is used in this process is selected for its ability to grow in tissue culture and for an absence of antibody synthesis. In contrast to polyclonal antibodies, which are mixtures of many different antibody molecules, the monoclonal antibodies produced by each hybridoma line are all chemically identical.

Interleukin 5 (IL5) is an interleukin produced by type-2 T helper cells and mast cells.
Theralizumab is an immunomodulatory drug developed by Thomas Hünig of the University of Würzburg. It was withdrawn from development after inducing severe inflammatory reactions as well as chronic organ failure in the first-in-human study by PAREXEL in London in March 2006. The developing company, TeGenero Immuno Therapeutics, went bankrupt later that year. The commercial rights were then acquired by a Russian startup, TheraMAB. The drug was renamed TAB08. Phase I and II clinical trials have been completed for arthritis and clinical trials have been initiated for cancer.
Humanized antibodies are antibodies from non-human species whose protein sequences have been modified to increase their similarity to antibody variants produced naturally in humans. The process of "humanization" is usually applied to monoclonal antibodies developed for administration to humans. Humanization can be necessary when the process of developing a specific antibody involves generation in a non-human immune system. The protein sequences of antibodies produced in this way are partially distinct from homologous antibodies occurring naturally in humans, and are therefore potentially immunogenic when administered to human patients. The International Nonproprietary Names of humanized antibodies end in -zumab, as in omalizumab.
Muromonab-CD3 is an immunosuppressant drug given to reduce acute rejection in patients with organ transplants. It is a monoclonal antibody targeted at the CD3 receptor, a membrane protein on the surface of T cells. It was the first monoclonal antibody to be approved for clinical use in humans.
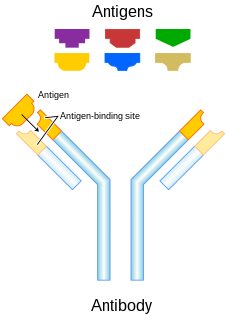
Monoclonal antibody therapy is a form of immunotherapy that uses monoclonal antibodies (mAbs) to bind monospecifically to certain cells or proteins. The objective is that this treatment will stimulate the patient's immune system to attack those cells. Alternatively, in radioimmunotherapy a radioactive dose localizes a target cell line, delivering lethal chemical doses. Antibodies have been used to bind to molecules involved in T-cell regulation to remove inhibitory pathways that block T-cell responses. This is known as immune checkpoint therapy.

Interleukin 20 (IL20) is a protein that is in humans encoded by the IL20 gene which is located in close proximity to the IL-10 gene on the 1q32 chromosome. IL-20 is a part of an IL-20 subfamily which is a part of a larger IL-10 family.
Technetium (99mTc) arcitumomab is a drug used for the diagnostic imaging of colorectal cancers, marketed by Immunomedics. It consists of the Fab' fragment of a monoclonal antibody and a radionuclide, technetium-99m.
Inolimomab is a mouse monoclonal antibody developed as an immunosuppressive drug against graft-versus-host disease. Its target is the alpha chain of the interleukin-2 receptor.
Visilizumab is a humanized monoclonal antibody. It is being investigated for use as an immunosuppressive drug in patients with ulcerative colitis and Crohn's disease. Visilizumab binds to the CD3 receptor on certain activated T cells without affecting resting T cells. It is currently under clinical studies for the treatment of ulcerative colitis and Crohn's disease.
Tanox was a biopharmaceutical company based in Houston, Texas. The company was founded by two biomedical research scientists, Nancy T. Chang and Tse Wen Chang in March 1986 with $250,000, which was a large part of their family savings at that time. Both Changs grew up and received college education in chemistry in National Tsing Hua University in Taiwan and obtained Ph.D. degrees from Harvard University. For postdoctoral training, Tse Wen shifted to immunology and did research with Herman N. Eisen at the Center for Cancer Research, M.I.T. The two Changs successively became research managers and worked with a range of monoclonal antibody projects in Centocor, Inc. based in Malvern, Pennsylvania, from 1981 to 1985. The Changs were recruited by Baylor College of Medicine toward the end of 1985 and offered faculty positions in the Division of Molecular Virology. Soon after their arrival, they were encouraged by a high-ranking Baylor official and local business leaders to start a biotech venture in Houston. This was in a period of time when the economy of Houston was in slump as the result of the collapse of the oil industry.

Interleukin 6 receptor (IL6R) also known as CD126 is a type I cytokine receptor.
Milatuzumab is an anti-CD74 humanized monoclonal antibody for the treatment of multiple myeloma non-Hodgkin's lymphoma and chronic lymphocytic leukemia.
Siltuximab is a chimeric monoclonal antibody. It binds to interleukin-6. Siltuximab has been investigated for the treatment of neoplastic diseases: metastatic renal cell cancer, prostate cancer, and Castleman's disease, among other types of cancer.
A rabbit hybridoma is a hybrid cell line formed by the fusion of an antibody producing rabbit B cell with a cancerous B-cell (myeloma).
MDX-1097 is a monoclonal antibody therapy being assessed in Phase IIb clinical trials as a treatment for multiple myeloma, a type of white blood cell cancer. It is a chimeric version of the mouse monoclonal antibody K-1-21. MDX-1097 targets kappa free immunoglobulin light chains which are found on the surface of some kappa light chain-restricted myeloma cells.
Dinutuximab and dinutuximab beta are monoclonal antibodies used as a second-line treatment for children with high-risk neuroblastoma. Each antibody is made of both mouse and human components and targets glycolipid GD2, expressed on neuroblastoma cells and on normal cells of neuroectodermal origin, including the central nervous system and peripheral nerves. They differ in that dinutuximab is manufactured using mouse cells, and dinutuximab beta is manufactured using hamster cells. The dosing regime differs, and dinutuximab is given in combination with granulocyte-macrophage colony stimulating factor (GM-CSF), interleukin-2 (IL-2) and 13-cis-retinoic acid (RA), while dinutuximab beta can be given alone.
Camidanlumab tesirine is an antibody-drug conjugate (ADC) composed of a human antibody that binds to the protein CD25, conjugated to a pyrrolobenzodiazepine dimer toxin. The experimental drug, developed by ADC Therapeutics is being tested in clinical trials for the treatment of B-cell Hodgkin's lymphoma (HL) and non-Hodgkin lymphoma (NHL), and for the treatment of B-cell acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML).