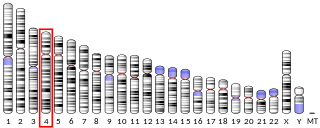
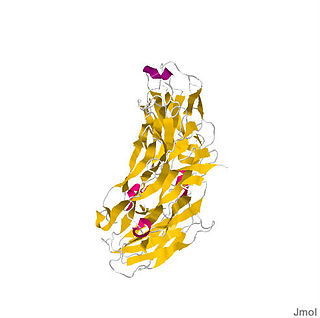
Interleukin-17A is a protein that in humans is encoded by the IL17A gene. In rodents, IL-17A used to be referred to as CTLA8, after the similarity with a viral gene ( O40633 ). [5] [6]
Interleukin-17A is a protein that in humans is encoded by the IL17A gene. In rodents, IL-17A used to be referred to as CTLA8, after the similarity with a viral gene ( O40633 ). [5] [6]
The protein encoded by this gene is a proinflammatory cytokine produced by activated T cells. This cytokine regulates the activities of NF-kappaB and mitogen-activated protein kinases. This cytokine can stimulate the expression of IL6 and cyclooxygenase-2 (PTGS2/COX-2), as well as enhance the production of nitric oxide (NO).
IL-17A, often referred to as IL-17, was originally discovered at transcriptional level by Rouvier et al. in 1993 from a rodent T-cell hybridoma, derived from the fusion of a mouse cytotoxic T cell clone and a rat T cell lymphoma. [5] Human and mouse IL-17A were cloned a few years later by Yao [7] and Kennedy. [8] Lymphocytes including CD4+, CD8+, gamma-delta T (γδ-T), invariant NKT and innate lymphoid cells (ILCs) are primary sources of IL-17A. [9] Non-T cells, such as neutrophils, have also been reported to produce IL-17A under certain circumstances. [10] IL-17A producing T helper cells (Th17 cells) are a distinct lineage from the Th1 and Th2 CD4+ lineages and the differentiation of Th17 cells requires STAT3 [11] and RORC. [12] IL-17A receptor A (IL-17RA) was first isolated and cloned from mouse EL4 thymoma cells and the bioactivity of IL-17A was confirmed by stimulating the transcriptional factor NF-kappa B activity and interleukin-6 (IL-6) secretion in fibroblasts. [13] IL-17RA pairs with IL-17RC to allow binding and signaling of IL-17A and IL-17F. [14]
High levels of this cytokine are associated with several chronic inflammatory diseases including rheumatoid arthritis, psoriasis and multiple sclerosis. [6]
Multiple sclerosis (MS) is a neurological disease caused by immune cells, which attack and destroy the myelin sheath that insulates neurons in the brain and spinal cord. This disease and its animal model experimental autoimmune encephalomyelitis (EAE) have historically been associated with the discovery of Th17 cells. [15] [16] However, elevated expression of IL-17A in multiple sclerosis (MS) lesions as well as peripheral blood has been documented before the identification of Th17 cells. [17] [18] Human TH17 cells have been shown to efficiently transmigrate across the blood-brain barrier in multiple sclerosis lesions, promoting central nervous system inflammation. [19]
Psoriasis is an auto-inflammatory skin disease characterized by circumscribed, crimson red, silver-scaled, plaque-like inflammatory lesions. Initially, psoriasis was considered to be a Th1-mediated disease since elevated levels of IFN-γ, TNF-α, and IL-12 was found in the serum and lesions of psoriasis patients. [20] However, the finding of IL-17-producing cells as well as IL17A transcripts in the lesions of psoriatic patients suggested that Th17 cells may synergize with Th1 cells in driving the pathology in psoriasis. [21] [22] The levels of IL-17A in the synovium correlate with tissue damage, whereas levels of IFN-γ correlate with protection. [23] Direct clinical significance of IL-17A in RA comes from recent clinical trials which found that two anti-IL-17A antibodies, namely secukinumab and ixekizumab significantly benefit these patients. [24] [25]
Th17 cells is also strongly associated rheumatoid arthritis (RA), a chronic disorder with symptoms include chronic joint inflammation, autoantibody production, which lead to the destruction of cartilage and bone. [26]
Th17 cells and IL-17 have also been linked to Crohn's disease (CD) and ulcerative colitis (UC), the two main forms of inflammatory bowel diseases (IBD). Th17 cells infiltrate massively to the inflamed tissue of IBD patients and both in vitro and in vivo studies have shown that Th17-related cytokines may initiate and amplify multiple pro-inflammatory pathways. [27] Elevated IL-17A levels in IBD have been reported by several groups. [28] [29] Nonetheless, Th17 signature cytokines, such as IL-17A and IL-22, may target gut epithelial cells and promote the activation of regulatory pathways and confer protection in the gastrointestinal tract. [30] [31] To this end, recent clinical trials targeting IL-17A in IBD were negative and actually showed increased adverse events in the treatment arm. [32] This data raised the question regarding the role of IL-17A in IBD pathogenesis and suggested that the elevated IL-17A might be beneficial for IBD patients.
Systemic lupus erythematosus, commonly referred as SLE or lupus, is a complex immune disorder affects the skin, joints, kidneys, and brain. Although the exact cause of lupus is not fully known, it has been reported that IL-17 and Th17 cells are involved in disease pathogenesis. [33] It has been reported that serum IL-17 levels are also elevated in SLE patients compared to controls [34] [35] and the Th17 pathway has been shown to drive autoimmune responses in pre-clinical mouse models of lupus. [36] [37] More importantly, IL-17- and IL-17-producing cells have also been detected in kidney tissue and skin biopsies from SLE patients. [38] [39] [40]
Elevated levels of IL-17A have been found in the sputum and in bronchoalveolar lavage fluid of patients with asthma [41] and a positive correlation between IL-17A production and asthma severity has been established. [42] In murine models, treatment with dexamethasone inhibits the release of Th2-related cytokines but does not affect IL-17A production. [43] Furthermore, Th17 cell-mediated airway inflammation and airway hyperresponsiveness are steroid resistant, indicating a potential role for Th17 cells in steroid-resistant asthma. [43] However, a recent trial using anti-IL-17RA did not show efficacy in subjects with asthma. [44]
Recent studies have suggested the involvement of immunological mechanisms in COPD. [45] An increase in Th17 cells was observed in patients with COPD compared with current smokers without COPD and healthy subjects, and inverse correlations were found between Th17 cells with lung function. [46] Gene expression profiling of bronchial brushings obtained from COPD patients also linked lung function to several Th17 signature genes such as SAA1, SAA2, SLC26A4 and LCN2. [47] Animal studies have shown that cigarette smoke promotes pathogenic Th17 differentiation and induces emphysema, [48] while blocking IL-17A using neutralizing antibody significantly decreased neutrophil recruitment and the pathological score of airway inflammation in tobacco-smoke-exposed mice. [48] [49]
In host defense, IL-17A has been shown to be mostly beneficial against infection caused by extracellular bacteria and fungi. [50] The primary function of Th17 cells appears to be control of the gut microbiota [51] [52] as well as the clearance of extracellular bacteria and fungi. IL-17A and IL-17 receptor signaling has been shown to be play a protective role in host defenses against many bacterial and fungal pathogens including Klebsiella pneumoniae, Mycoplasma pneumoniae, Candida albicans, Coccidioides posadasii, Histoplasma capsulatum, and Blastomyces dermatitidis. [53] However, IL-17A seems to be detrimental in viral infection such as influenza through promoting neutrophilic inflammation. [54]
The requirements of IL-17A and IL-17 receptor signaling in host defense were well documented and appreciated before the identification of Th17 cells as an independent T helper cell lineage. In experimental pneumonia models, IL-17A or IL-17RA knock mice have increased susceptibility to various Gram-negative bacteria, such as Klebsiella pneumoniae [55] and Mycoplasma pneumoniae. [56] In contrast, data suggest that IL-23 and IL-17A are not required for protection against primary infection by the intracellular bacteria Mycobacterium tuberculosis. Both the IL-17RA knock out mice and the IL-23p19 knock out mice cleared primary infection with M. tuberculosis. [57] [58] However, IL-17A is required for protection against primary infection with a different intracellular bacteria, Francisella tularensis. [59]
Mouse model studies using the IL-17RA knock out mice and the IL-17A knock out mice with the murine adapted influenza strain (PR8) [54] as well as the 2009 pandemic H1N1 strain [93] both support that IL-17A plays a detrimental role in mediating the acute lung injury. [60]
The role of adaptive immune responses mediated by antigen specific Th17 has been investigated more recently. Antigen specific Th17 cells were also shown to recognize conserved protein antigens among different K. pneumoniae strains and provide broad-spectrum serotype-independent protection. [61] Antigen specific CD4 T cells also limit nasopharyngeal colonization of S. pneumoniae in mouse models. [62] Furthermore, immunization with pneumococcal whole cell antigen and several derivatives provided IL-17-mediated, but not antibody dependent, protection against S. pneumoniae challenge. [63] [64] In fungal infection, it has been shown an IL-17 producing clone with a TCR specific for calnexin from Blastomyces dermatitidis confers protection with evolutionary related fungal species including Histoplasma spp. [65]
In tumorigenesis, IL-17A has been shown to recruit myeloid derived suppressor cells (MDSCs) to dampen anti-tumor immunity. [66] [67] IL-17A can also enhance tumor growth in vivo through the induction of IL-6, which in turn activates oncogenic transcription factor signal transducer and activator of transcription 3 (STAT3) and upregulates pro-survival and pro-angiogenic genes in tumors. [68] The exact role of IL-17A in angiogenesis has yet to be determined and current data suggest that IL-17A can promote or suppress tumor development. [69] IL-17A seemed to facilitate development of colorectal carcinoma by fostering angiogenesis via promote VEGF production from cancer cells [70] and it has been shown that IL-17A also mediates tumor resistance to anti-VEGF therapy through the recruitment of MDSCs. [71]
However IL-17A KO mice were more susceptible to developing metastatic lung melanoma, [72] suggesting that IL-17A can possibly promote the production of the potent antitumor cytokine IFN-γ, produced by cytotoxic T cells. Indeed, data from ovarian cancer suggest that Th17 cells are positively correlated with NK cell–mediated immunity and anti-tumor CD8 responses. [73]
The presence of IL-17 has been proven in a number of ocular diseases associated with neovascularization. Elevated concentration of IL-17 have been shown in vitreous fluid during proliferative diabetic retinopathy. Increased rates of Th17 cells and higher concentrations of IL-17 have been observed in patients with age-related macular degeneration. [74]
The discovery of the key roles of IL-17A and IL-17A producing cells in inflammation, autoimmune diseases and host defense has led to the experimental targeting of the IL-17A pathway in animal models of diseases as well as in clinical trials in humans. Targeting IL-17A has been proven to be a good approach as anti-IL-17A is FDA approved for the treatment of psoriasis in 2015. [75]
Secukinumab (anti-IL-17A) has been evaluated in psoriasis and the first report showing Secukinumab is effective when compared with placebo was published in 2010. [76] In 2015, the US Food and Drug Administration (FDA) and European Medicines Agency (EMA) approved anti-IL-17 for the treatment of psoriasis. [77]
Other than the monoclonal antibodies, highly specific and potent inhibitors targeting Th17 specific transcription factor RORγt have been identified and found to be highly effective. [78]
Vitamin D, a potent immunomodulator, has also been shown to suppress Th17 cell differentiation and function by several research groups. [79] The active form of vitamin D has been found to 'severely impair' [80] production of the IL17 and IL-17F cytokines by Th17 cells.
The 2017 version of this article was updated by an external expert under a dual publication model. The corresponding academic peer reviewed article was published in Gene and can be cited as: Kong Chen; Jay K Kolls (22 January 2017). "Interluekin-17A (IL17A)". Gene . Gene Wiki Review Series. 614: 8–14. doi:10.1016/J.GENE.2017.01.016. ISSN 0378-1119. PMC 5394985 . PMID 28122268. Wikidata Q39103136. |

Interleukin 10 (IL-10), also known as human cytokine synthesis inhibitory factor (CSIF), is an anti-inflammatory cytokine. In humans, interleukin 10 is encoded by the IL10 gene. IL-10 signals through a receptor complex consisting of two IL-10 receptor-1 and two IL-10 receptor-2 proteins. Consequently, the functional receptor consists of four IL-10 receptor molecules. IL-10 binding induces STAT3 signalling via the phosphorylation of the cytoplasmic tails of IL-10 receptor 1 + IL-10 receptor 2 by JAK1 and Tyk2 respectively.

Interleukin-23 subunit alpha is a protein that in humans is encoded by the IL23A gene. The protein is also known as IL-23p19. It is one of the two subunits of the cytokine Interleukin-23.
Interleukin 21 (IL-21) is a protein that in humans is encoded by the IL21 gene.

Interleukin-26 (IL-26) is a protein that in humans is encoded by the IL26 gene.

Interleukin-25 (IL-25) – also known as interleukin-17E (IL-17E) – is a protein that in humans is encoded by the IL25 gene on chromosome 14. IL-25 was discovered in 2001 and is made up of 177 amino acids.

Interleukin 24 (IL-24) is a protein in the interleukin family, a type of cytokine signaling molecule in the immune system. In humans, this protein is encoded by the IL24 gene.

Interleukin-22 (IL-22) is protein that in humans is encoded by the IL22 gene.

Interleukin 20 (IL20) is a protein that is in humans encoded by the IL20 gene which is located in close proximity to the IL-10 gene on the 1q32 chromosome. IL-20 is a part of an IL-20 subfamily which is a part of a larger IL-10 family.

Interleukin 17 family is a family of pro-inflammatory cystine knot cytokines. They are produced by a group of T helper cell known as T helper 17 cell in response to their stimulation with IL-23. Originally, Th17 was identified in 1993 by Rouvier et al. who isolated IL17A transcript from a rodent T-cell hybridoma. The protein encoded by IL17A is a founding member of IL-17 family. IL17A protein exhibits a high homology with a viral IL-17-like protein encoded in the genome of T-lymphotropic rhadinovirus Herpesvirus saimiri. In rodents, IL-17A is often referred to as CTLA8.

Signal transducer and activator of transcription 4 (STAT4) is a transcription factor belonging to the STAT protein family, composed of STAT1, STAT2, STAT3, STAT4, STAT5A, STAT5B, STAT6. STAT proteins are key activators of gene transcription which bind to DNA in response to cytokine gradient. STAT proteins are a common part of Janus kinase (JAK)- signalling pathways, activated by cytokines.STAT4 is required for the development of Th1 cells from naive CD4+ T cells and IFN-γ production in response to IL-12. There are two known STAT4 transcripts, STAT4α and STAT4β, differing in the levels of interferon-gamma production downstream.
T helper 17 cells (Th17) are a subset of pro-inflammatory T helper cells defined by their production of interleukin 17 (IL-17). They are related to T regulatory cells and the signals that cause Th17s to differentiate actually inhibit Treg differentiation. However, Th17s are developmentally distinct from Th1 and Th2 lineages. Th17 cells play an important role in maintaining mucosal barriers and contributing to pathogen clearance at mucosal surfaces; such protective and non-pathogenic Th17 cells have been termed as Treg17 cells.
Interleukin 35 (IL-35) is a recently discovered anti-inflammatory cytokine from the IL-12 family. Member of IL-12 family - IL-35 is produced by wide range of regulatory lymphocytes and plays a role in immune suppression. IL-35 can block the development of Th1 and Th17 cells by limiting early T cell proliferation.

The interleukin-23 receptor is a type I cytokine receptor. It is encoded in human by the IL23R gene. In complex with the interleukin-12 receptor β1 subunit (IL-12Rβ1), it is activated by the cytokine interleukin 23 (IL-23). The IL23R mRNA is 2.8 kilobases in length and includes 12 exons. The translated protein contains 629 amino acids; it is a type I penetrating protein and includes a signal peptide, an N-terminal fibronectin III-like domain and an intracellular part that contains three potential tyrosine phosphorylation domains. There are 24 IL23R splice variants in mitogen-activated lymphocytes. IL23R includes some single-nucleotide polymorphisms in the region encoding the domain that binds IL-23, which may lead to differences between people in Th17 activation. There is also a variant of IL-23R that consists of just the extracellular part and is known as soluble IL-23R. This form can compete with the membrane-bound form to bind IL-23, modulating the Th17 immune response and regulation of inflammation and immune function.
Interleukin-17 receptor (IL-17R) is a cytokine receptor which belongs to new subfamily of receptors binding proinflammatory cytokine interleukin 17A, a member of IL-17 family ligands produced by T helper 17 cells (Th17). IL-17R family consists of 5 members: IL-17RA, IL-17RB, IL-17RC, IL-17RD and IL-17RE. Functional IL-17R is a transmembrane receptor complex usually consisting of one IL-17RA, which is a founding member of the family, and second other family subunit, thus forming heteromeric receptor binding different ligands. IL-17A, a founding member of IL-17 ligand family binds to heteromeric IL-17RA/RC receptor complex. IL-17RB binds preferentially IL-17B and IL-17E and heteromeric IL-17RA/RE complex binds IL-17C. However, there is still unknown ligand for IL-17RD. The first identified member IL-17RA is located on human chromosome 22, whereas other subunits IL-17RB to IL-17RD are encoded within human chromosome 3.

The Interleukin-1 family is a group of 11 cytokines that plays a central role in the regulation of immune and inflammatory responses to infections or sterile insults.

Interleukin 23 (IL-23) is a heterodimeric cytokine composed of an IL-12B (IL-12p40) subunit and an IL-23A (IL-23p19) subunit. IL-23 is part of the IL-12 family of cytokines. The functional receptor for IL-23 consists of a heterodimer between IL-12Rβ1 and IL-23R.
Regulatory B cells (Bregs or Breg cells) represent a small population of B cells that participates in immunomodulation and in the suppression of immune responses. The population of Bregs can be further separated into different human or murine subsets such as B10 cells, marginal zone B cells, Br1 cells, GrB+B cells, CD9+ B cells, and even some plasmablasts or plasma cells. Bregs regulate the immune system by different mechanisms. One of the main mechanisms is the production of anti-inflammatory cytokines such as interleukin 10 (IL-10), IL-35, or transforming growth factor beta (TGF-β). Another known mechanism is the production of cytotoxic Granzyme B. Bregs also express various inhibitory surface markers such as programmed death-ligand 1 (PD-L1), CD39, CD73, and aryl hydrocarbon receptor. The regulatory effects of Bregs were described in various models of inflammation, autoimmune diseases, transplantation reactions, and in anti-tumor immunity.
In cell biology, TH9 cells are a sub-population of CD4+T cells that produce interleukin-9 (IL-9). They play a role in defense against helminth infections, in allergic responses, in autoimmunity, and tumor suppression.

Type 3 innate lymphoid cells (ILC3) are immune cells from the lymphoid lineage that are part of the innate immune system. These cells participate in innate mechanisms on mucous membranes, contributing to tissue homeostasis, host-commensal mutualism and pathogen clearance. They are part of a heterogeneous group of innate lymphoid cells, which is traditionally divided into three subsets based on their expression of master transcription factors as well as secreted effector cytokines - ILC1, ILC2 and ILC3.

Interleukin 17F (IL-17F) is signaling protein that is in human is encoded by the IL17F gene and is considered a pro-inflammatory cytokine. This protein belongs to the interleukin 17 family and is mainly produced by the T helper 17 cells after their stimulation with interleukin 23. However, IL-17F can be also produced by a wide range of cell types, including innate immune cells and epithelial cells.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.