| |
 | |
| Clinical data | |
|---|---|
| Trade names | Sprycel, Dasanix |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a607063 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth (tablets) |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 96% |
| Metabolism | Liver |
| Elimination half-life | 1.3 to 5 hours |
| Excretion | Fecal (85%), kidney (4%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.228.321 |
| Chemical and physical data | |
| Formula | C22H26ClN7O2S |
| Molar mass | 488.01 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Dasatinib, sold under the brand name Sprycel among others, is a targeted therapy medication used to treat certain cases of chronic myelogenous leukemia (CML) and acute lymphoblastic leukemia (ALL). [3] Specifically it is used to treat cases that are Philadelphia chromosome-positive (Ph+). [3] It is taken by mouth. [3]
Contents
- Medical uses
- Adverse effects
- Pharmacology
- History
- Society and culture
- Legal status
- Economics
- Brand names
- Research
- Dasatinib+Quercetin
- References
- Further reading
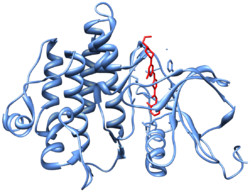
Common adverse effects include low white blood cells, low blood platelets, anemia, swelling, rash, and diarrhea. [3] Severe adverse effects may include bleeding, pulmonary edema, heart failure, and prolonged QT syndrome. [3] Use during pregnancy may result in harm to the fetus. [3] It is a tyrosine-kinase inhibitor and works by blocking a number of tyrosine kinases such as Bcr-Abl and the Src kinase family. [3]
Dasatinib was approved for medical use in the United States and in the European Union in 2006. [3] [2] It is on the World Health Organization's List of Essential Medicines. [4]