| Fatty liver | |
|---|---|
| Synonyms | Fatty liver disease (FLD), hepatic steatosis, simple steatosis |
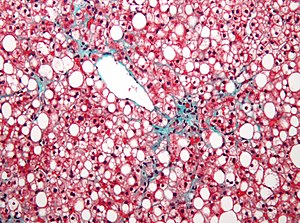 | |
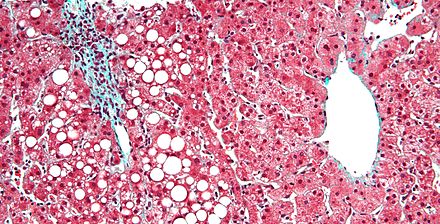
| Micrograph showing a fatty liver (macrovesicular steatosis), as seen in non-alcoholic fatty liver disease. Trichrome stain. | |
| Specialty | Gastroenterology |
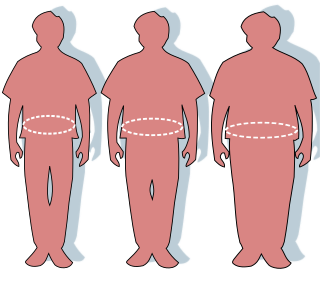
Fatty liver , or hepatic steatosis or simple steatosis, is a reversible condition wherein large vacuoles of triglyceride fat accumulate in liver cells via the process of steatosis (i.e., abnormal retention of lipids within a cell). Despite having multiple causes, fatty liver can be considered a single disease that occurs worldwide in those with excessive alcohol intake and the obese (with or without effects of insulin resistance). The condition is also associated with other diseases that influence fat metabolism. [1] When this process of fat metabolism is disrupted, the fat can accumulate in the liver in excessive amounts, thus resulting in a fatty liver. [2] It is difficult to distinguish alcoholic FLD, which is part of alcoholic liver disease, from nonalcoholic FLD (NAFLD), and both show microvesicular and macrovesicular fatty changes at different stages.

The liver, an organ only found in vertebrates, detoxifies various metabolites, synthesizes proteins, and produces biochemicals necessary for digestion. In humans, it is located in the right upper quadrant of the abdomen, below the diaphragm. Its other roles in metabolism include the regulation of glycogen storage, decomposition of red blood cells and the production of hormones.

A vacuole is a membrane-bound organelle which is present in all plant and fungal cells and some protist, animal and bacterial cells. Vacuoles are essentially enclosed compartments which are filled with water containing inorganic and organic molecules including enzymes in solution, though in certain cases they may contain solids which have been engulfed. Vacuoles are formed by the fusion of multiple membrane vesicles and are effectively just larger forms of these. The organelle has no basic shape or size; its structure varies according to the requirements of the cell.

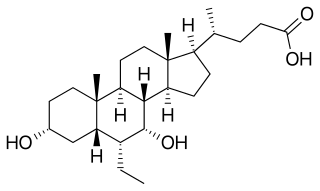
A triglyceride is an ester derived from glycerol and three fatty acids. Triglycerides are the main constituents of body fat in humans and other animals, as well as vegetable fat. They are also present in the blood to enable the bidirectional transference of adipose fat and blood glucose from the liver, and are a major component of human skin oils.
Contents
- Signs and symptoms
- Complications
- Causes
- Pathology
- Diagnosis
- Treatment
- Epidemiology
- See also
- References
- External links
The accumulation of fat in alcoholic or non-alcoholic steatosis may also be accompanied by a progressive inflammation of the liver (hepatitis), called steatohepatitis. This more severe condition may be termed either alcoholic steatohepatitis or non-alcoholic steatohepatitis (NASH).

Hepatitis is inflammation of the liver tissue. Some people have no symptoms whereas others develop yellow discoloration of the skin and whites of the eyes, poor appetite, vomiting, tiredness, abdominal pain, or diarrhea. Hepatitis may be temporary (acute) or long term (chronic) depending on whether it lasts for less than or more than six months. Acute hepatitis can sometimes resolve on its own, progress to chronic hepatitis, or rarely result in acute liver failure. Over time the chronic form may progress to scarring of the liver, liver failure, or liver cancer.

Steatohepatitis is a type of fatty liver disease, characterized by inflammation of the liver with concurrent fat accumulation in liver. Mere deposition of fat in the liver is termed steatosis, and together these constitute fatty liver changes.