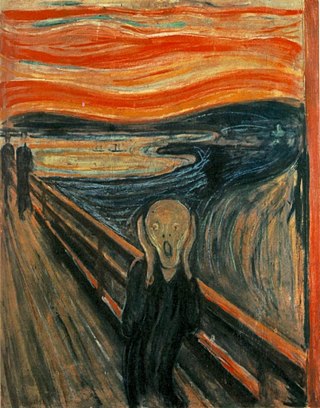
Anxiety is an emotion which is characterised by an unpleasant state of inner turmoil and includes feelings of dread over anticipated events. Anxiety is different from fear in that fear is defined as the emotional response to a present threat, whereas anxiety is the anticipation of a future one. It is often accompanied by nervous behavior such as pacing back and forth, somatic complaints, and rumination.

Cognitive behavioral therapy (CBT) is a form of psychotherapy that aims to reduce symptoms of various mental health conditions, primarily depression, PTSD and anxiety disorders. Cognitive behavioral therapy focuses on challenging and changing cognitive distortions and their associated behaviors to improve emotional regulation and develop personal coping strategies that target solving current problems. Though it was originally designed to treat depression, its uses have been expanded to include many issues and the treatment of many mental health and other conditions, including anxiety, substance use disorders, marital problems, ADHD, and eating disorders. CBT includes a number of cognitive or behavioral psychotherapies that treat defined psychopathologies using evidence-based techniques and strategies.

A mental disorder is an impairment of the mind disrupting normal thinking, feeling, mood, behavior, or social interactions, and accompanied by significant distress or dysfunction. The causes of mental disorders are very complex and vary depending on the particular disorder and the individual. Although the causes of most mental disorders are not fully understood, researchers have identified a variety of biological, psychological, and environmental factors that can contribute to the development or progression of mental disorders. Most mental disorders result in a combination of several different factors rather than just a single factor.
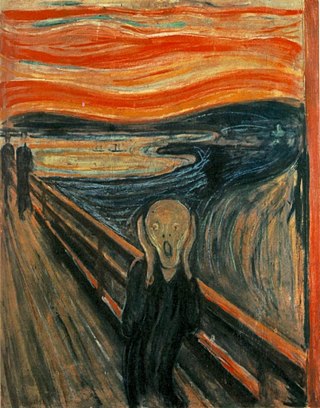
Anxiety disorders are a group of mental disorders characterized by significant and uncontrollable feelings of anxiety and fear such that a person's social, occupational, and personal functions are significantly impaired. Anxiety may cause physical and cognitive symptoms, such as restlessness, irritability, easy fatigue, difficulty concentrating, increased heart rate, chest pain, abdominal pain, and a variety of other symptoms that may vary based on the individual.
Post-traumatic stress disorder (PTSD) is a mental and behavioral disorder that develops from experiencing a traumatic event, such as sexual assault, warfare, traffic collisions, child abuse, domestic violence, or other threats on a person's life or well-being. Symptoms may include disturbing thoughts, feelings, or dreams related to the events, mental or physical distress to trauma-related cues, attempts to avoid trauma-related cues, alterations in the way a person thinks and feels, and an increase in the fight-or-flight response. These symptoms last for more than a month after the event and can include triggers such as misophonia. Young children are less likely to show distress, but instead may express their memories through play. A person with PTSD is at a higher risk of suicide and intentional self-harm.

Stress, whether physiological, biological or psychological, is an organism's response to a stressor such as an environmental condition. When stressed by stimuli that alter an organism's environment, multiple systems respond across the body. In humans and most mammals, the autonomic nervous system and hypothalamic-pituitary-adrenal (HPA) axis are the two major systems that respond to stress. Two well-known hormones that humans produce during stressful situations are adrenaline and cortisol.

Depression is a mental state of low mood and aversion to activity. It affects about 3.5% of the global population, or about 280 million people of all ages. Depression affects a person's thoughts, behavior, feelings, and sense of well-being. Experiences that would normally bring a person pleasure or joy give reduced pleasure or joy, and the afflicted person often experiences a loss of motivation or interest in those activities.

Social support is the perception and actuality that one is cared for, has assistance available from other people, and most popularly, that one is part of a supportive social network. These supportive resources can be emotional, informational, or companionship ; tangible or intangible. Social support can be measured as the perception that one has assistance available, the actual received assistance, or the degree to which a person is integrated in a social network. Support can come from many sources, such as family, friends, pets, neighbors, coworkers, organizations, etc.
Child psychopathology refers to the scientific study of mental disorders in children and adolescents. Oppositional defiant disorder, attention-deficit hyperactivity disorder, and autism spectrum disorder are examples of psychopathology that are typically first diagnosed during childhood. Mental health providers who work with children and adolescents are informed by research in developmental psychology, clinical child psychology, and family systems. Lists of child and adult mental disorders can be found in the International Statistical Classification of Diseases and Related Health Problems, 10th Edition (ICD-10), published by the World Health Organization (WHO) and in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association (APA). In addition, the Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood is used in assessing mental health and developmental disorders in children up to age five.
Childhood trauma is often described as serious adverse childhood experiences (ACEs). Children may go through a range of experiences that classify as psychological trauma; these might include neglect, abandonment, sexual abuse, emotional abuse, and physical abuse. They may also witness abuse of a sibling or parent, or have a mentally ill parent. These events can have profound psychological, physiological, and sociological impacts leading to lasting negative effects on health and well-being. These events may include antisocial behaviors, attention deficit hyperactivity disorder (ADHD), and sleep disturbances. Additionally, children whose mothers have experienced traumatic or stressful events during pregnancy have an increased risk of mental health disorders and other neurodevelopmental disorders.
Caregiver syndrome or caregiver stress is a condition that strongly manifests exhaustion, anger, rage, or guilt resulting from unrelieved caring for a chronically ill patient. This condition is not listed in the United States' Diagnostic and Statistical Manual of Mental Disorders, although the term is often used by many healthcare professionals in that country. The equivalent used in many other countries, the ICD-11, does include the condition.

The ICD-11 of the World Health Organization (WHO) describes occupational burnout as an occupational phenomenon resulting from chronic workplace stress that has not been successfully managed, with symptoms characterized by "feelings of energy depletion or exhaustion; increased mental distance from one’s job, or feelings of negativism or cynicism related to one's job; and reduced professional efficacy." It is classified as a mismatch between the challenges of work and a person's mental and physical resources, but is not recognized by the WHO as a medical condition.

Occupational stress is psychological stress related to one's job. Occupational stress refers to a chronic condition. Occupational stress can be managed by understanding what the stressful conditions at work are and taking steps to remediate those conditions. Occupational stress can occur when workers do not feel supported by supervisors or coworkers, feel as if they have little control over the work they perform, or find that their efforts on the job are incommensurate with the job's rewards. Occupational stress is a concern for both employees and employers because stressful job conditions are related to employees' emotional well-being, physical health, and job performance. The World Health Organization and the International Labour Organization conducted a study. The results showed that exposure to long working hours, operates through increased psycho-social occupational stress. It is the occupational risk factor with the largest attributable burden of disease, according to these official estimates causing an estimated 745,000 workers to die from ischemic heart disease and stroke events in 2016.

In psychology, stress is a feeling of emotional strain and pressure. Stress is a type of psychological pain. Small amounts of stress may be beneficial, as it can improve athletic performance, motivation and reaction to the environment. Excessive amounts of stress, however, can increase the risk of strokes, heart attacks, ulcers, and mental illnesses such as depression and also aggravation of a pre-existing condition.
Minority stress describes high levels of stress faced by members of stigmatized minority groups. It may be caused by a number of factors, including poor social support and low socioeconomic status; well understood causes of minority stress are interpersonal prejudice and discrimination. Indeed, numerous scientific studies have shown that when minority individuals experience a high degree of prejudice, this can cause stress responses that accrue over time, eventually leading to poor mental and physical health. Minority stress theory summarizes these scientific studies to explain how difficult social situations lead to chronic stress and poor health among minority individuals.
Childbirth-related post-traumatic stress disorder is a psychological disorder that can develop in women who have recently given birth. This disorder can also affect men or partners who have observed a difficult birth. Its symptoms are not distinct from post-traumatic stress disorder (PTSD). It may also be called post-traumatic stress disorder following childbirth (PTSD-FC).
Marriage and health are closely related. Married people experience lower morbidity and mortality across such diverse health threats as cancer, heart attacks, and surgery. There are gender differences in these effects which may be partially due to men's and women's relative status. Most research on marriage and health has focused on heterosexual couples, and more work is needed to clarify the health effects on same-sex marriage. Simply being married, as well as the quality of one's marriage, has been linked to diverse measures of health. Research has examined the social-cognitive, emotional, behavioral and biological processes involved in these links.

The effects of climate change on mental health and wellbeing are being documented as the consequences of climate change become more tangible and impactful. This is especially the case for vulnerable populations and those with pre-existing serious mental illness. There are three broad pathways by which these effects can take place: directly, indirectly or via awareness. The direct pathway includes stress-related conditions caused by exposure to extreme weather events. These include post-traumatic stress disorder (PTSD). Scientific studies have linked mental health to several climate-related exposures. These include heat, humidity, rainfall, drought, wildfires and floods. The indirect pathway can be disruption to economic and social activities. An example is when an area of farmland is less able to produce food. The third pathway can be of mere awareness of the climate change threat, even by individuals who are not otherwise affected by it. This especially manifests in the form of anxiety over the quality of life for future generations.
Attachment and health is a psychological model which considers how the attachment theory pertains to people's preferences and expectations for the proximity of others when faced with stress, threat, danger or pain. In 1982, American psychiatrist Lawrence Kolb noticed that patients with chronic pain displayed behaviours with their healthcare providers akin to what children might display with an attachment figure, thus marking one of the first applications of the attachment theory to physical health. Development of the adult attachment theory and adult attachment measures in the 1990s provided researchers with the means to apply the attachment theory to health in a more systematic way. Since that time, it has been used to understand variations in stress response, health outcomes and health behaviour. Ultimately, the application of the attachment theory to health care may enable health care practitioners to provide more personalized medicine by creating a deeper understanding of patient distress and allowing clinicians to better meet their needs and expectations.

The COVID-19 pandemic has impacted the mental health of people across the globe. The pandemic has caused widespread anxiety, depression, and post-traumatic stress disorder symptoms. According to the UN health agency WHO, in the first year of the COVID-19 pandemic, prevalence of common mental health conditions, such as depression and anxiety, went up by more than 25 percent. The pandemic has damaged social relationships, trust in institutions and in other people, has caused changes in work and income, and has imposed a substantial burden of anxiety and worry on the population. Women and young people face the greatest risk of depression and anxiety. According to The Centers for Disease Control and Prevention study of Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic, "63 percent of young people reported experiencing substantial symptoms of anxiety and depression".