Signs and symptoms
| | This section is empty. You can help by adding to it. (October 2021) |
| Anorectal varices | |
|---|---|
| Specialty | Gastroenterology, Hematology |
| Symptoms | Coffee ground vomiting, Hematochezia |
| Complications | Internal bleeding, hypovolemic shock, cardiac arrest |
| Causes | Portal hypertension |
| Treatment | Treating portal hypertension, surgery (transjugular intrahepatic portosystemic shunt) |
Anorectal varices are collateral submucosal blood vessels dilated by backflow in the veins of the rectum. [1] Typically this occurs due to portal hypertension which shunts venous blood from the portal system through the portosystemic anastomosis present at this site into the systemic venous system. [2] [3] This can also occur in the esophagus, causing esophageal varices, and at the level of the umbilicus, causing caput medusae. [4] Between 44% and 78% of patients with portal hypertension get anorectal varices. [3] [5]
| | This section is empty. You can help by adding to it. (October 2021) |
Blood from the superior portion of the rectum normally drains into the superior rectal vein and via the inferior mesenteric vein to the liver as part of the portal venous system. Blood from the middle and inferior portions of the rectum is drained via the middle and inferior rectal veins. In portal hypertension, venous resistance is increased within the portal venous system; when the pressure in the portal venous system increases above that of the systemic, blood is shunted through the portosystemic anastomoses. The shunting of blood and consequential increase of pressure through the collateral veins causes the varicosities.[ citation needed ]
The terms rectal varices and haemorrhoids are often used interchangeably, but this is not correct. [6] Haemorrhoids are due to prolapse of the rectal venous plexus and are no more common in patients with portal hypertension than `in those without. [7] Rectal varices, however, are found only in patients with portal hypertension and are common in conditions such as cirrhosis. [8]
Unlike esophageal varices, rectal varices are less prone to bleeding, are less serious when a bleed does occur, and are easier to treat because of the more accessible location. [9] However, in some cases, rectal varices can result in severe bleeding. [10]
Typically, treatment consists of addressing the underlying portal hypertension. Some treatments include portosystemic shunting, ligation, and under-running suturing. [5] Insertion of a transjugular intrahepatic portosystemic shunt (TIPS) has been shown to alleviate varices caused by portal hypertension. [1] Successful treatment of portal hypertension that subsequently reduces anorectal varices provides a confirmation of the initial diagnosis, allowing for a distinction between varices and hemorrhoids, which would not have been alleviated by reduction of portal hypertension.[ citation needed ]
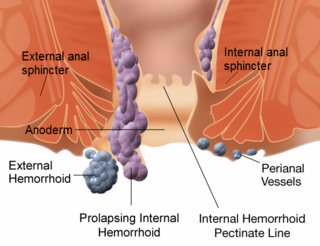
Hemorrhoids, also known as piles, are vascular structures in the anal canal. In their normal state, they are cushions that help with stool control. They become a disease when swollen or inflamed; the unqualified term hemorrhoid is often used to refer to the disease. The signs and symptoms of hemorrhoids depend on the type present. Internal hemorrhoids often result in painless, bright red rectal bleeding when defecating. External hemorrhoids often result in pain and swelling in the area of the anus. If bleeding occurs, it is usually darker. Symptoms frequently get better after a few days. A skin tag may remain after the healing of an external hemorrhoid.

Ascites is the abnormal build-up of fluid in the abdomen. Technically, it is more than 25 ml of fluid in the peritoneal cavity, although volumes greater than one liter may occur. Symptoms may include increased abdominal size, increased weight, abdominal discomfort, and shortness of breath. Complications can include spontaneous bacterial peritonitis.

In medicine, a shunt is a hole or a small passage that moves, or allows movement of, fluid from one part of the body to another. The term may describe either congenital or acquired shunts; acquired shunts may be either biological or mechanical.

Budd–Chiari syndrome is a very rare condition, affecting one in a million adults. The condition is caused by occlusion of the hepatic veins that drain the liver. The symptoms are non-specific and vary widely, but it may present with the classical triad of abdominal pain, ascites, and liver enlargement. It is usually seen in younger adults, with the median age at diagnosis between the ages of 35 and 40, and it has a similar incidence in males and females. The syndrome can be fulminant, acute, chronic, or asymptomatic. Subacute presentation is the most common form.

Esophageal varices are extremely dilated sub-mucosal veins in the lower third of the esophagus. They are most often a consequence of portal hypertension, commonly due to cirrhosis. People with esophageal varices have a strong tendency to develop severe bleeding which left untreated can be fatal. Esophageal varices are typically diagnosed through an esophagogastroduodenoscopy.
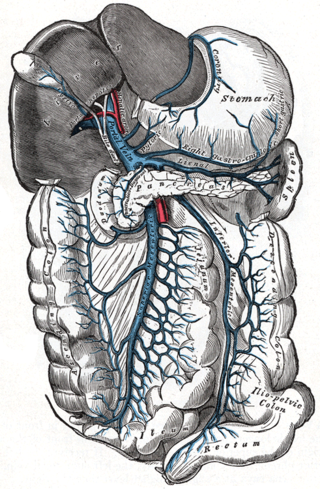
Portal hypertension is defined as increased portal venous pressure, with a hepatic venous pressure gradient greater than 5 mmHg. Normal portal pressure is 1–4 mmHg; clinically insignificant portal hypertension is present at portal pressures 5–9 mmHg; clinically significant portal hypertension is present at portal pressures greater than 10 mmHg. The portal vein and its branches supply most of the blood and nutrients from the intestine to the liver.

Gastrointestinal bleeding, also called gastrointestinal hemorrhage (GIB), is all forms of bleeding in the gastrointestinal tract, from the mouth to the rectum. When there is significant blood loss over a short time, symptoms may include vomiting red blood, vomiting black blood, bloody stool, or black stool. Small amounts of bleeding over a long time may cause iron-deficiency anemia resulting in feeling tired or heart-related chest pain. Other symptoms may include abdominal pain, shortness of breath, pale skin, or passing out. Sometimes in those with small amounts of bleeding no symptoms may be present.

Gastric varices are dilated submucosal veins in the lining of the stomach, which can be a life-threatening cause of bleeding in the upper gastrointestinal tract. They are most commonly found in patients with portal hypertension, or elevated pressure in the portal vein system, which may be a complication of cirrhosis. Gastric varices may also be found in patients with thrombosis of the splenic vein, into which the short gastric veins that drain the fundus of the stomach flow. The latter may be a complication of acute pancreatitis, pancreatic cancer, or other abdominal tumours, as well as hepatitis C. Gastric varices and associated bleeding are a potential complication of schistosomiasis resulting from portal hypertension.

Caput medusae is the appearance of distended and engorged superficial epigastric veins, which are seen radiating from the umbilicus across the abdomen. The name caput medusae originates from the apparent similarity to Medusa's head, which had venomous snakes in place of hair. It is also a sign of portal hypertension. When the portal vein, that transfers the blood from the gastrointestinal tract to the liver, is blocked, the blood volume increases in the peripheral blood vessels making them appear engorged. It is caused by dilation of the paraumbilical veins, which carry oxygenated blood from mother to fetus in utero and normally close within one week of birth, becoming re-canalised due to portal hypertension caused by liver failure.The appearance is due to cutanous portosystemic collateral formation between distended and engorged paraumbilical veins that radiate from the umbilicus across the abdomen to join systemic veins.

Transjugular intrahepatic portosystemic shunt is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein. It is used to treat portal hypertension which frequently leads to intestinal bleeding, life-threatening esophageal bleeding and the buildup of fluid within the abdomen (ascites).

Portal vein thrombosis (PVT) is a vascular disease of the liver that occurs when a blood clot occurs in the hepatic portal vein, which can lead to increased pressure in the portal vein system and reduced blood supply to the liver. The mortality rate is approximately 1 in 10.

Gastric antral vascular ectasia (GAVE) is an uncommon cause of chronic gastrointestinal bleeding or iron deficiency anemia. The condition is associated with dilated small blood vessels in the gastric antrum, which is a distal part of the stomach. The dilated vessels result in intestinal bleeding. It is also called watermelon stomach because streaky long red areas that are present in the stomach may resemble the markings on watermelon.

In medicine, a distal splenorenal shunt procedure (DSRS), also splenorenal shunt procedure and Warren shunt, is a surgical procedure in which the distal splenic vein is attached to the left renal vein. It is used to treat portal hypertension and its main complication. It was developed by W. Dean Warren.

The rectal venous plexus is the venous plexus surrounding the rectum. It consists of an internal and an external rectal plexus. It is drained by the superior, middle, and inferior rectal veins. It forms a portosystemic (portocaval) anastomosis. This allows rectally administered medications to bypass first pass metabolism.
A portacaval anastomosis or portocaval anastomosis is a specific type of circulatory anastomosis that occurs between the veins of the portal circulation and the vena cava, thus forming one of the principal types of portasystemic anastomosis or portosystemic anastomosis, as it connects the portal circulation to the systemic circulation, providing an alternative pathway for the blood. When there is a blockage of the portal system, portocaval anastomosis enables the blood to still reach the systemic venous circulation. The inferior end of the esophagus and the superior part of the rectum are potential sites of a harmful portocaval anastomosis.
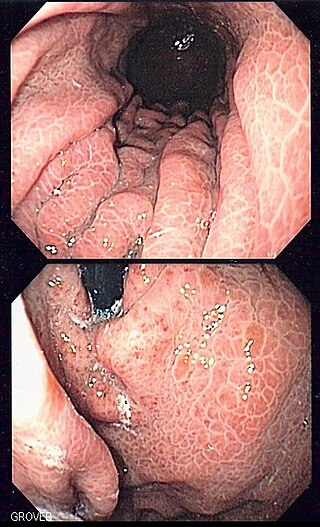
Portal hypertensive gastropathy refers to changes in the mucosa of the stomach in patients with portal hypertension; by far the most common cause of this is cirrhosis of the liver. These changes in the mucosa include friability of the mucosa and the presence of ectatic blood vessels at the surface. Patients with portal hypertensive gastropathy may experience bleeding from the stomach, which may uncommonly manifest itself in vomiting blood or melena; however, portal hypertension may cause several other more common sources of upper gastrointestinal bleeding, such as esophageal varices and gastric varices. On endoscopic evaluation of the stomach, this condition shows a characteristic mosaic or "snake-skin" appearance to the mucosa of the stomach.
Portal venous pressure is the blood pressure in the hepatic portal vein, and is normally between 5-10 mmHg. Raised portal venous pressure is termed portal hypertension, and has numerous sequelae such as ascites and hepatic encephalopathy.
The Sugiura procedure is a surgical technique that involves the removal and transection of the blood vessels that supply the upper portion of the stomach and the esophagus. The procedure also involves a splenectomy. The operation was originally developed to treat bleeding esophageal varices that were untreatable by other conventional methods. It was originally developed as a two-step operation, but has been modified numerous times by many surgeons since its original creation.
Congenital portosystemic shunts (PSS) is a hereditary condition in dogs and cats, its frequency varying depending on the breed. The shunts found mainly in small dog breeds such as Shih Tzus, Tibetan Spaniels, Miniature Schnauzers and Yorkshire Terriers, and in cats such as Persians, British Shorthairs, Himalayans, and mixed breeds are usually extrahepatic, while the shunts found in large dog breeds such as Irish Wolfhounds and Labrador Retrievers tend to be intrahepatic.
Balloon-occluded retrograde transvenous obliteration (BRTO) is an endovascular procedure used for the treatment of gastric varices. When performing the procedure, an interventional radiologist accesses blood vessels using a catheter, inflates a balloon and injects a substance into the variceal blood vessels that causes blockage of those vessels. To prevent the flow of the agent out of the intended site, a balloon is inflated during the procedure, which occludes.