| Familial cirrhosis | |
|---|---|
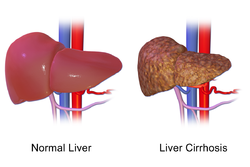 | |
| Liver Cirrhosis. | |
| Specialty | Hepatology |
Familial cirrhosis is a form of liver disease that is inherited and the liver scarring is not caused by any obvious disease process. This type of cirrhosis is a keratin disease. Damage progresses until function becomes impaired.[ citation needed ]
Contents
Current cirrhosis treatment is aimed at managing complications as well as chronic poor health related to liver damage. Treatments include abstinence from alcohol, nutritional supplement, identification of any identifiable disease process, management of portal hypertension, and liver transplantation.[ citation needed ]