Chlamydophila (1999–2009)
Earlier criteria for differentiation of chlamydial species did not always work well. For example, at that time C. psittaci was distinguished from C. trachomatis by sulfadiazine resistance, although not all strains identified as C. psittaci at the time were resistant, and C. pneumoniae was classified by its appearance under electron microscopy (EM) and its ability to infect humans, although the EM appearance may differ from one research group to the next, and many of these species infected humans.
A major re-description of the Chlamydiales order in 1999, using the then-new techniques of DNA analysis split three of the species from the genus Chlamydia and reclassified them in the then newly created genus Chlamydophila (Cp. thereafter). Five new species were added by splitting from existing species: [7]
Summary of 1999 Classification change [8] | Old name | Host | New name |
|---|
| C. psittaci | Birds | Cp. psittaci |
| Mammals | Cp. abortus |
| Cats | Cp. felis |
| Guinea pig | Cp. caviae |
| C. pecorum | Mammals | Cp. pecorum |
| C. pneumoniae | Humans | Cp. pneumoniae |
| C. trachomatis | Humans | C. trachomatis |
| Swine | C. suis |
| Mice and hamsters | C. muridarum |
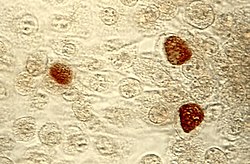
According to the authors of the 1999 study, the mean DNA–DNA reassociation difference distinguishing Chlamydophila from Chlamydia is 10.1%, an accepted value for genus separation. Although the 16S ribosomal RNA gene sequences of the two are close to 95% identical, unlike the other previously established genera, the authors considered a less than 95% similarity only a guideline for establishing new genera in chlamydial families. In the study, the authors used the similarity of the locations of coding for protein and ribosomal RNA genes in the genome (gene clusters) to help distinguish Chlamydophila from Chlamydia. Also, the full-length 23S ribosomal RNA genes of the species of the two genera were less than 95% identical. [7] Supporting criteria such as antigen detection, [9] glycogen staining, host association, and EM morphology were also employed, depending on applicability and availability.
Some molecular criteria distinguishing Chlamydiaceae genera [7] | Genus | Approximate genome size (Mega base pairs) | Detectable glycogen | Number of rDNA operons |
|---|
| Chlamydophila | 1.2 | No | 1 |
|---|
| Chlamydia | 1.0 | Yes | 2 |
|---|
In 2001 many bacteriologists strongly objected to the reclassification. [1] Comparative genomic analyses in 2006 identified a number of signature proteins that were uniquely present in species from the genera Chlamydia and Chlamydophila, which supported the distinctness of Chlamydophila, but did not support an "early separation" scenario as suggested by rRNA. [10]
In 2009 the validity of Chlamydophila was challenged by newer DNA analysis techniques (using 100 concatenated proteins instead of 16S rRNA), leading to a proposal to "reunite the Chlamydiaceae into a single genus, Chlamydia". The authors pointed to the poor bootstrap support of the 1999 rRNA tree, which demonstrated a split in only 68% of the sampled trees, and argued that the 2006 study did not provide sufficiently-strong support for the separation. [11] This reversion appears to have been accepted by the community [12] and was formally validated in 2015, [13] [14] bringing the number of (valid) Chlamydia species up to 9 as of 2017. [15] The merger of the genus Chlamydophila back into the genus Chlamydia is, by 2018, generally accepted. [16] [17] [18] [19]
However, the much newer analyses of Genome Taxonomy Database using 120 concatenated proteins again show a split of those two genera to be valid (see § Phylogeny below), and has lead to the resurrection of the genus in the GTDB and GBIF taxonomies. [20] [21] Joseph et al. 2015, which proposed new species from strains formerly known as C. psittaci, also recovered a coherent Chlamydophila clade in their whole-genome tree, but with an unusual topology showing Chlamydophila to be sister to C. muridarum. [5] Gupta et al. (2015) finds 1 CSI + 19 CSPs specific for Chlamydophilia and 2 CSIs + 19 CSPs specific for the three-species version of Chlamydia. [22]