Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.

The coccyx, commonly referred to as the tailbone, is the final segment of the vertebral column in all apes, and analogous structures in certain other mammals such as horses. In tailless primates since Nacholapithecus, the coccyx is the remnant of a vestigial tail. In animals with bony tails, it is known as tailhead or dock, in bird anatomy as tailfan. It comprises three to five separate or fused coccygeal vertebrae below the sacrum, attached to the sacrum by a fibrocartilaginous joint, the sacrococcygeal symphysis, which permits limited movement between the sacrum and the coccyx.

A teratoma is a tumor made up of several types of tissue, such as hair, muscle, teeth, or bone. Teratomata typically form in the tailbone, ovary, or testicle.

A rhabdomyoma is a benign tumor of striated muscle. Rhabdomyomas may be either cardiac or extracardiac. Extracardiac forms of rhabdomyoma are sub-classified into three distinct types: adult type, fetal type, and genital type.

Germ cell tumor (GCT) is a neoplasm derived from the primordial germ cells. Germ-cell tumors can be cancerous or benign. Germ cells normally occur inside the gonads. GCTs that originate outside the gonads may be birth defects resulting from errors during development of the embryo.

Hydrops fetalis or hydrops foetalis is a condition in the fetus characterized by an accumulation of fluid, or edema, in at least two fetal compartments. By comparison, hydrops allantois or hydrops amnion is an accumulation of excessive fluid in the allantoic or amniotic space, respectively.

Hemangioendotheliomas are a family of vascular neoplasms of intermediate malignancy.

Fetal surgery, also known as antenatal surgery or prenatal surgery, is a growing branch of maternal-fetal medicine that covers any of a broad range of surgical techniques that are used to treat congenital abnormalities in fetuses who are still in the pregnant uterus. There are three main types: open fetal surgery, which involves completely opening the uterus to operate on the fetus; minimally invasive fetoscopic surgery, which uses small incisions and is guided by fetoscopy and sonography; and percutaneous fetal therapy, which involves placing a catheter under continuous ultrasound guidance.

The EXIT procedure, or ex utero intrapartum treatment procedure, is a specialized surgical delivery procedure used to deliver babies who have airway compression. Causes of airway compression in newborn babies result from a number of rare congenital disorders, including bronchopulmonary sequestration, congenital cystic adenomatoid malformation, mouth or neck tumor such as teratoma, and lung or pleural tumor such as pleuropulmonary blastoma. Airway compression discovered at birth is a medical emergency. In many cases, however, the airway compression is discovered during prenatal ultrasound exams, permitting time to plan a safe delivery using the EXIT procedure or other means.
A cystic hygroma is a form of lymphatic malformation. It is an abnormal growth that usually appears on a baby's neck or head. It consists of one or more cysts and tends to grow larger over time. The disorder usually develops while the fetus is still in the uterus, but can also appear after birth.

Perineal hernia is a hernia involving the perineum. The hernia may contain fluid, fat, any part of the intestine, the rectum, or the bladder. It is known to occur in humans, dogs, and other mammals, and often appears as a sudden swelling to one side of the anus.

Primary tumors of the heart are extremely rare tumors that arise from the normal tissues that make up the heart. The incidence of primary cardiac tumors has been found to be approximately 0.02%. This is in contrast to secondary tumors of the heart, which are typically either metastatic from another part of the body, or infiltrate the heart via direct extension from the surrounding tissues. Metastatic tumors to the heart are about 20 times more common than primary cardiac tumors.

Currarino syndrome is an inherited congenital disorder where either the sacrum is not formed properly, or there is a mass in the presacral space in front of the sacrum, and there are malformations of the anus or rectum. It occurs in approximately 1 in 100,000 people.

Maternal–fetal medicine (MFM), also known as perinatology, is a branch of medicine that focuses on managing health concerns of the mother and fetus prior to, during, and shortly after pregnancy.

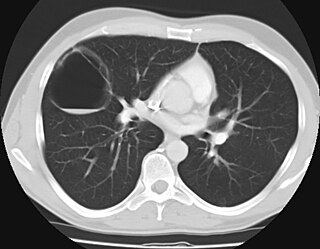
Pulmonary hypoplasia is an incomplete development of the lungs, resulting in an abnormally low number or small size of bronchopulmonary segments or alveoli. A congenital malformation, most often occurs secondary to other fetal abnormalities that interfere with normal development of the lungs. Primary (idiopathic) pulmonary hypoplasia is rare and usually not associated with other maternal or fetal abnormalities.
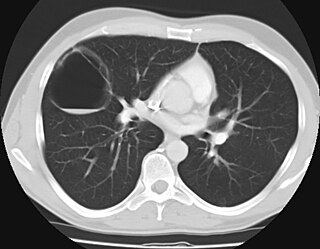
Congenital pulmonary airway malformation (CPAM), formerly known as congenital cystic adenomatoid malformation (CCAM), is a congenital disorder of the lung similar to bronchopulmonary sequestration. In CPAM, usually an entire lobe of lung is replaced by a non-working cystic piece of abnormal lung tissue. This abnormal tissue will never function as normal lung tissue. The underlying cause for CPAM is unknown. It occurs in approximately 1 in every 30,000 pregnancies.
Elevated alpha-fetoprotein refers to a state where alpha-fetoprotein levels are outside of the reference range.

Scrotalultrasound is a medical ultrasound examination of the scrotum. It is used in the evaluation of testicular pain, and can help identify solid masses.
Congenital varicella syndrome is a rare disease resulting from Varicella Zoster virus (VZV) infection during the period of gestation. Viremia during the primary infection can result in transplacental transmission of the infection to the developing fetus. An estimated 25% of fetuses get infected with varicella infection when mother has a varicella infection during the pregnancy but the risk of developing congenital varicella syndrome is around 2%, therefore majority of the outcomes are normal newborns. Patients with primary infection before 20 weeks of gestation are at a higher risk of developing the severe form of infection, affecting the eyes, limbs, skin and the central nervous system. Diagnosis requires a documented history of primary infection in the mother and serial ultrasound demonstrating features suggestive of congenital varicella syndrome. There is no definitive treatment, termination of pregnancy in fetuses with severe features is recommended. Vaccination to prevent maternal varicella infection and proper counseling to avoid contact with infected people are important for the management options to reduce the incidence of congenital varicella syndrome.
Epignathus is a rare teratoma of the oropharynx. Epignathus is a form of oropharyngeal teratoma that arises from the palate and, in most cases, results in death. The pathology is thought to be due to unorganized and uncontrolled differentiation of somatic cells leading to formation of the teratoma; sometimes it is also referred to as fetus in fetu, which is an extremely rare occurrence of an incomplete but parasitic fetus located in the body of its twin. This tumor is considered benign (non-cancerous) but life-threatening because of its atypical features and high risk of airway obstruction, which is the cause of death in 80-100% of the cases at the time of delivery.