Serotonin–norepinephrine reuptake inhibitors (SNRIs) are a class of antidepressant medications used to treat major depressive disorder (MDD), anxiety disorders, social phobia, chronic neuropathic pain, fibromyalgia syndrome (FMS), and menopausal symptoms. Off-label uses include treatments for attention-deficit hyperactivity disorder (ADHD), and obsessive–compulsive disorder (OCD). SNRIs are monoamine reuptake inhibitors; specifically, they inhibit the reuptake of serotonin and norepinephrine. These neurotransmitters are thought to play an important role in mood regulation. SNRIs can be contrasted with the selective serotonin reuptake inhibitors (SSRIs) and norepinephrine reuptake inhibitors (NRIs), which act upon single neurotransmitters.
A dopamine reuptake inhibitor (DRI) is a class of drug which acts as a reuptake inhibitor of the monoamine neurotransmitter dopamine by blocking the action of the dopamine transporter (DAT). Reuptake inhibition is achieved when extracellular dopamine not absorbed by the postsynaptic neuron is blocked from re-entering the presynaptic neuron. This results in increased extracellular concentrations of dopamine and increase in dopaminergic neurotransmission.

A norepinephrine reuptake inhibitor or noradrenaline reuptake inhibitor or adrenergic reuptake inhibitor (ARI), is a type of drug that acts as a reuptake inhibitor for the neurotransmitters norepinephrine (noradrenaline) and epinephrine (adrenaline) by blocking the action of the norepinephrine transporter (NET). This in turn leads to increased extracellular concentrations of norepinephrine and epinephrine and therefore can increase adrenergic neurotransmission.
A spontaneous orgasm, or spontaneous ejaculation when it occurs in males, is an orgasm which occurs spontaneously and involuntarily without sexual stimulation. Nocturnal emissions may be considered a normal/physiological form of spontaneous orgasm. Pathological spontaneous orgasms can be experienced as pleasurable, non-pleasurable, or unpleasant, and can be distressing. Causes of pathological spontaneous orgasms include spinal cord lesions, psychological causes, rabies, and medications. Some cases may have no identifiable cause. Spontaneous orgasms may have no trigger or may be triggered by various non-sexual circumstances. They may occur in both males and females. Treatment of spontaneous orgasms include psychotherapy, selective serotonin reuptake inhibitors (SSRIs), the alpha-1 blocker silodosin, and anxiolytics.

A serotonin reuptake inhibitor (SRI) is a type of drug which acts as a reuptake inhibitor of the neurotransmitter serotonin by blocking the action of the serotonin transporter (SERT). This in turn leads to increased extracellular concentrations of serotonin and, therefore, an increase in serotonergic neurotransmission. It is a type of monoamine reuptake inhibitor (MRI); other types of MRIs include dopamine reuptake inhibitors and norepinephrine reuptake inhibitors.

Seproxetine, also known as (S)-norfluoxetine, is a selective serotonin reuptake inhibitor (SSRI). It is the S enantiomer of norfluoxetine, the main active metabolite of the widely used antidepressant fluoxetine; it is nearly 4 times more selective for stimulating neurosteroid synthesis relative to serotonin reuptake inhibition than fluoxetine. It is formed through the demethylation, or removal of a methyl group, of fluoxetine. Seproxetine is both an inhibitor of serotonin and dopamine transporters, 5-HT2A and 5-HT2C receptors. It was being investigated by Eli Lilly and Company as an antidepressant; however, it inhibited the KvLQT1 protein, which is responsible for the management of the QT interval. This is the time it takes for the heart to contract and recover. Due to the inhibition, the QT interval was prolonged, which could lead to significant cardiac side complications. Due to this, development of the medication was discontinued. Tests on its efficacy found that it was equivalent to fluoxetine, but sixteen times more powerful than the R enantiomer of norfluoxetine.
Reuptake inhibitors (RIs) are a type of reuptake modulators. It is a drug that inhibits the plasmalemmal transporter-mediated reuptake of a neurotransmitter from the synapse into the pre-synaptic neuron. This leads to an increase in extracellular concentrations of the neurotransmitter and an increase in neurotransmission. Various drugs exert their psychological and physiological effects through reuptake inhibition, including many antidepressants and psychostimulants.

Vilazodone, sold under the brand name Viibryd among others, is a medication used to treat major depressive disorder. It is classified as a serotonin modulator and is taken by mouth.

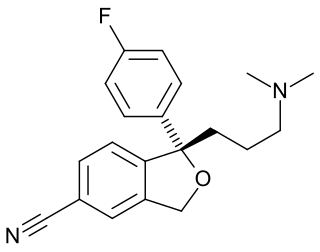
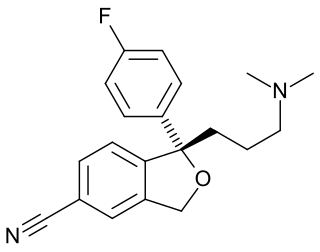
Talopram, also known as phthalapromine, is a selective norepinephrine reuptake inhibitor (NRI) which was researched for the management of depression in the 1960s and 1970s but was never commercialized. Along with talsupram, talopram is structurally related to the selective serotonin reuptake inhibitor (SSRI) citalopram, as well as to melitracen:
In 1971, the company hired Klaus Bøgesø as a medicinal chemist. Over the years Bøgesø turned out to have a Midas touch at the game of drug hunting, creating more molecules that made it to the market than almost any other medicinal chemist in the field. The challenge facing him in 1971 following his recruitment was to produce a selective norepinephrine reuptake inhibitor. Like other companies at the time, Lundbeck had little interest in an SSRI. Bøgesø began from an accident in the laboratory. Trying to create a derivative of their norepinephrine reuptake inhibiting antidepressant melitracen, Lundbeck chemists accidentally produced a new chemical — a phenylphthalene. Against all the odds, just like melitracen, this was also a selective norepinephrine reuptake inhibitor. Two potential antidepressants came out of this — talopram and tasulopram, which were pressed into clinical trials. Both however turned out to be energizing, and in a number of cases there were suicide attempts. The fact that there were suicide attempts appeared to confirm another proposal of Paul Kielholz, that activating antidepressants might lead to suicide. Lundbeck's experience suggested that norepinephrine reuptake inhibitors were likely to lead to just this problem. Lundbeck retreated, scared. If norepinephrine reuptake inhibitors were likely to trigger suicide, the greatest hazard of an antidepressant, then Kielholz's view suggested that an SSRI would be less likely to lead to suicide. Bøgesø's job was to see whether the new series of drugs could be converted into a series of SSRIs. Following a lead from Carlsson on how to do this, he converted talopram into citalopram, the most selective serotonin reuptake inhibitor to come to the market.

SB-649,915 is a serotonin reuptake inhibitor and 5-HT1A and 5-HT1B receptor antagonist which is being investigated for its antidepressant effects. Relative to the selective serotonin reuptake inhibitors (SSRIs), SB-649,915 has a faster onset of action and may also have greater clinical efficacy as well. This can be attributed to blockade of 5-HT1A and 5-HT1B autoreceptors which inhibit serotonin release.

Lubazodone is an experimental antidepressant which was under development by Yamanouchi for the treatment for major depressive disorder in the late 1990s and early 2000s but was never marketed. It acts as a serotonin reuptake inhibitor and 5-HT2A receptor antagonist, and hence has the profile of a serotonin antagonist and reuptake inhibitor (SARI). The drug has good selectivity against a range of other monoamine receptors, with its next highest affinities being for the α1-adrenergic receptor and the 5-HT2C receptor. Lubazodone is structurally related to trazodone and nefazodone, but is a stronger serotonin reuptake inhibitor and weaker as a 5-HT2A receptor antagonist in comparison to them and is more balanced in its actions as a SARI. It reached phase II clinical trials for depression, but development was discontinued in 2001 reportedly due to the "erosion of the SSRITooltip selective serotonin reuptake inhibitor market in the United States".

Desmethylsertraline (DMS), also known as norsertraline, is an active metabolite of the antidepressant drug sertraline. Like sertraline, desmethylsertraline acts as a monoamine reuptake inhibitor, and may be responsible for some of its parent's therapeutic benefits; however, the effects of DMS's main activity of increasing serotonin levels via binding to the serotonin transporter appears to be negligible as in vivo testing showed no measurable change in brain activity despite a nearly 20-fold increase in DMS blood levels compared to the EC50 (i.e. the amount required to achieve the desired effect in 50% of the population) of its parent drug sertraline. DMS is significantly less potent relative to sertraline as a serotonin reuptake inhibitor (Ki = 76 nM vs. 3 nM, respectively), but conversely, is more balanced as a monoamine reuptake inhibitor (5-HT (Ki) = 76 nM; NE (Ki) = 420 nM; DA (Ki) = 440 nM), which has the effective result of DMS contrarily behaving as a serotonin-norepinephrine-dopamine reuptake inhibitor (SNDRI), with about 5.5-fold preference for inhibiting serotonin reuptake relative to catecholamine reuptake.

JZ-IV-10 is a piperidine derivative related to cocaine which acts as a highly potent serotonin–norepinephrine–dopamine reuptake inhibitor. The eugeroic modafinil was used as a lead to fuel this compound's discovery.

Selective serotonin reuptake inhibitors (SSRIs) are a class of drugs that are typically used as antidepressants in the treatment of major depressive disorder, anxiety disorders, and other psychological conditions.

Ifoxetine (CGP-15,210-G) is a selective serotonin reuptake inhibitor (SSRI) which was investigated as an antidepressant in the 1980s but was never marketed. Ifoxetine selectively blocks the reuptake of serotonin in the brain supposedly without affecting it in the periphery. Supporting this claim, ifoxetine was found to be efficacious in clinical trials and was very well tolerated, producing almost no physical side effects or other complaints of significant concern.

A serotonin–dopamine reuptake inhibitor (SDRI) is a type of drug which acts as a reuptake inhibitor of the monoamine neurotransmitters serotonin and dopamine by blocking the actions of the serotonin transporter (SERT) and dopamine transporter (DAT), respectively. This in turn leads to increased extracellular concentrations of serotonin and dopamine, and, therefore, an increase in serotonergic and dopaminergic neurotransmission.
A monoamine reuptake inhibitor (MRI) is a drug that acts as a reuptake inhibitor of one or more of the three major monoamine neurotransmitters serotonin, norepinephrine, and dopamine by blocking the action of one or more of the respective monoamine transporters (MATs), which include the serotonin transporter (SERT), norepinephrine transporter (NET), and dopamine transporter (DAT). This in turn results in an increase in the synaptic concentrations of one or more of these neurotransmitters and therefore an increase in monoaminergic neurotransmission.
A serotonin modulator and stimulator (SMS), sometimes referred to more simply as a serotonin modulator, is a type of drug with a multimodal action specific to the serotonin neurotransmitter system. To be precise, SMSs simultaneously modulate one or more serotonin receptors and inhibit the reuptake of serotonin. The term was created to describe the mechanism of action of the serotonergic antidepressant vortioxetine, which acts as a serotonin reuptake inhibitor (SRI), agonist of the 5-HT1A receptor, and antagonist of the 5-HT3 and 5-HT7 receptors. However, it can also technically be applied to vilazodone, which is an antidepressant as well and acts as an SRI and 5-HT1A receptor partial agonist.

Cericlamine is a potent and moderately selective serotonin reuptake inhibitor (SSRI) of the amphetamine family that was investigated as an antidepressant for the treatment of depression, anxiety disorders, and anorexia nervosa by Jouveinal but did not complete development and was never marketed. It reached phase III clinical trials in 1996 before development was discontinued in 1999.