 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Ornidyl, others |
| Other names | α-difluoromethylornithine, DFMO |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Routes of administration | intravenous, topical |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 100% (Intravenous) Negligible (topical) |
| Metabolism | Not metabolized |
| Elimination half-life | 8 hours |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
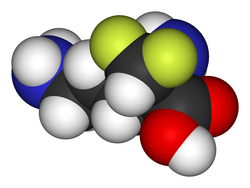
| Formula | C6H12F2N2O2 |
| Molar mass | 182.171 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Eflornithine, sold under the brand name Ornidyl among others, is a medication used to treat African trypanosomiasis (sleeping sickness) and excessive hair growth on the face in women. [1] [3] [4] Specifically it is used for the second stage of sleeping sickness caused by T. b. gambiense and may be used with nifurtimox. [3] [5] It is taken intravenously (injection into a vein) or topically. [3] [4] It is an ornithine decarboxylase inhibitor. [2]
Contents
- Medical uses
- Sleeping sickness
- Excess facial hair in women
- Neuroblastoma
- Contraindications
- Topical
- Oral administration
- Side effects
- Topical 2
- Intravenous
- Interactions
- Topical 3
- Mechanism of action
- Description
- Evidence
- Active site
- History
- Sleeping sickness treatment
- Society and culture
- Legal status
- Brand names
- Research
- Chemo preventative therapy
- Veterinary uses
- References
- External links
Common side effects when applied as a cream include rash, redness, and burning. [4] Side effects of the injectable form include bone marrow suppression, vomiting, and seizures. [5] It is unclear if it is safe to use during pregnancy or breastfeeding. [5] It is recommended typically for children over the age of 12. [5]
Eflornithine was developed in the 1970s and came into medical use in 1990. [6] It is on the World Health Organization's List of Essential Medicines. [7] In the United States the injectable form can be obtained from the US Centers for Disease Control and Prevention. [5] In regions of the world where sleeping sickness is common, eflornithine is provided for free by the World Health Organization. [8]




