Related Research Articles

α-Ketoglutaric acid is a dicarboxylic acid, i.e., a short-chain fatty acid containing two carboxyl groups with C, O, and H standing for carbon, oxygen, and hydrogen, respectively. However, almost all animal tissues and extracellular fluids have a pH above 7. At these basic pH levels α-ketoglutaric acid exists almost exclusively as its conjugate base. That is, it has two negative electric charges due to its release of positively charged hydrogen from both of its now negatively charged carboxy groups, CO−2. This double negatively charge molecule is referred to as α-ketoglutarate or 2-oxoglutarate.

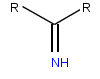
Butyric acid, also known under the systematic name butanoic acid, is a straight-chain alkyl carboxylic acid with the chemical formula CH3CH2CH2CO2H. It is an oily, colorless liquid with an unpleasant odor. Isobutyric acid is an isomer. Salts and esters of butyric acid are known as butyrates or butanoates. The acid does not occur widely in nature, but its esters are widespread. It is a common industrial chemical and an important component in the mammalian gut.

Ketogenesis is the biochemical process through which organisms produce ketone bodies by breaking down fatty acids and ketogenic amino acids. The process supplies energy to certain organs, particularly the brain, heart and skeletal muscle, under specific scenarios including fasting, caloric restriction, sleep, or others.

An antiporter is an integral membrane protein involved in secondary active transport. It is a type of cotransporter, which means that uses the movement of one In the case of an antiporter, two or more different molecules or ions are moved across a phospholipid membrane, such as the plasma membrane, in opposite directions, one into the cell and one out of the cell. This is in contrast to symporters, which are another type of cotransporter that moves two or more ions in the same direction.
Sodium-dependent glucose cotransporters are a family of glucose transporter found in the intestinal mucosa (enterocytes) of the small intestine (SGLT1) and the proximal tubule of the nephron. They contribute to renal glucose reabsorption. In the kidneys, 100% of the filtered glucose in the glomerulus has to be reabsorbed along the nephron. If the plasma glucose concentration is too high (hyperglycemia), glucose passes into the urine (glucosuria) because SGLT are saturated with the filtered glucose.

Sodium/glucose cotransporter 1 (SGLT1) also known as solute carrier family 5 member 1 is a protein in humans that is encoded by the SLC5A1 gene which encodes the production of the SGLT1 protein to line the absorptive cells in the small intestine and the epithelial cells of the kidney tubules of the nephron for the purpose of glucose uptake into cells. Recently, it has been seen to have functions that can be considered as promising therapeutic target to treat diabetes and obesity. Through the use of the sodium glucose cotransporter 1 protein, cells are able to obtain glucose which is further utilized to make and store energy for the cell.

Free fatty acid receptor 3 protein is a G protein coupled receptor that in humans is encoded by the FFAR3 gene. GPRs reside on cell surfaces, bind specific signaling molecules, and thereby are activated to trigger certain functional responses in their parent cells. FFAR3 is a member of the free fatty acid receptor group of GPRs that includes FFAR1, FFAR2, and FFAR4. All of these FFARs are activated by fatty acids. FFAR3 and FFAR2 are activated by certain short-chain fatty acids (SC-FAs), i.e., fatty acids consisting of 2 to 6 carbon atoms whereas FFFAR1 and FFAR4 are activated by certain fatty acids that are 6 to more than 21 carbon atoms long. Hydroxycarboxylic acid receptor 2 is also activated by a SC-FA that activate FFAR3, i.e., butyric acid.

Free fatty acid receptor 2 (FFAR2), also termed G-protein coupled receptor 43 (GPR43), is a rhodopsin-like G-protein coupled receptor. It is coded by the FFAR2 gene. In humans, the FFAR2 gene is located on the long arm of chromosome 19 at position 13.12. Like other GPCRs, FFAR2s reside on the surface membrane of cells and when bond to one of their activating ligands regulate the function of their parent cells. FFAR2 is a member of a small family of structurally and functionally related GPRs termed free fatty acid receptors (FFARs). This family includes three other receptors which, like FFAR2, are activated by certain fatty acids: FFAR1, FFAR3 (GPR41), and FFAR4 (GPR120). FFAR2 and FFAR3 are activated by short-chain fatty acids whereas FFAR1 and FFAR4 are activated by long-chain fatty acids.

Succinate receptor 1 (SUCNR1), previously named G protein-coupled receptor 91 (GPR91), is a receptor that is activated by succinate, i.e., the anionic form of the dicarboxylic acid, succinic acid. Succinate and succinic acid readily convert into each other by gaining (succinate) or losing (succinic acid) protons, i.e., H+ (see Ions). Succinate is by far the predominant form of this interconversion in living organisms. Succinate is one of the intermediate metabolites in the citric acid cycle (also termed the TCA cycle or tricarboxylic acid cycle). This cycle is a metabolic pathway that operates in the mitochondria of virtually all eucaryotic cells. It consists of a series of biochemical reactions that serve the vital function of releasing the energy stored in nutrient carbohydrates, fats, and proteins. Recent studies have found that some of the metabolites in this cycle are able to regulate various physiological and pathological functions in a wide range of cell types. The succinyl CoA in this cycle may release its bound succinate; succinate is one of these mitochondrial-formed bioactive metabolites.

Monocarboxylate transporter 5 is a protein that in humans is encoded by the SLC16A4 gene.

Monocarboxylate transporter 4 (MCT4) also known as solute carrier family 16 member 3 is a protein that in humans is encoded by the SLC16A3 gene.

Sodium-coupled monocarboxylate transporter 1 (i.e., SMCT1) and sodium-coupled monocarboxylate transporter 2 (i.e., SMCT2) are plasma membrane transport proteins in the solute carrier family. They transport sodium cations in association with the anionic forms (see conjugated base) of certain short-chain fatty acids (i.e., SC-FAs) through the plasma membrane from the outside to the inside of cells. For example, propionic acid (i.e., CH
3CH
2CO
2H) in its anionic "propionate" form (i.e., CH
3CH
2CO−
2) along with sodium cations (i.e., Na+) are co-transported from the extracellular fluid into a SMCT1-epxressing cell's cytoplasm. Monocarboxylate transporters (MCTs) are also transport proteins in the solute carrier family. They co-transport the anionic forms of various compounds into cells in association with proton cations (i.e. H+). Four of the 14 MCTs, i.e. SLC16A1 (i.e., MCT1), SLC16A7 (i.e., MCT22), SLC16A8 (i.e., MCT3), and SLC16A3 (i.e., MCT4), transport some of the same SC-FAs anions that the SMCTs transport into cells. SC-FAs do diffuse into cells independently of transport proteins but at the levels normally occurring in tissues far greater amounts of the SC-FAs are brought into cells that express a SC-FA transporter.

Monocarboxylate transporter 1 is a ubiquitous protein that in humans is encoded by the SLC16A1 gene. It is a proton coupled monocarboxylate transporter.
Iminoglycinuria is an autosomal recessive disorder of renal tubular transport affecting reabsorption of the amino acid glycine, and the imino acids proline and hydroxyproline. This results in excess urinary excretion of all three acids.
The monocarboxylate transporters, or MCTs, are a family of proton-linked plasma membrane transporters that carry molecules having one carboxylate group (monocarboxylates), such as lactate, pyruvate, and ketones across biological membranes. Acetate is actively transported to intestinal enteroendocrine cells via MCT, termed Targ. MCTs are expressed in nearly every kind of cell.

The organic anion transporter 1 (OAT1) also known as solute carrier family 22 member 6 (SLC22A6) is a protein that in humans is encoded by the SLC22A6 gene. It is a member of the organic anion transporter (OAT) family of proteins. OAT1 is a transmembrane protein that is expressed in the brain, the placenta, the eyes, smooth muscles, and the basolateral membrane of proximal tubular cells of the kidneys. It plays a central role in renal organic anion transport. Along with OAT3, OAT1 mediates the uptake of a wide range of relatively small and hydrophilic organic anions from plasma into the cytoplasm of the proximal tubular cells of the kidneys. From there, these substrates are transported into the lumen of the nephrons of the kidneys for excretion. OAT1 homologs have been identified in rats, mice, rabbits, pigs, flounders, and nematodes.

Monocarboxylate transporter 10, also known as aromatic amino acid transporter 1 and T-type amino acid transporter 1 (TAT1) and solute carrier family 16 member 10 (SLC16A10), is a protein that in humans is encoded by the SLC16A10 gene. SLC16A10 is a member of the solute carrier family.
The lactate shuttle hypothesis describes the movement of lactate intracellularly and intercellularly. The hypothesis is based on the observation that lactate is formed and utilized continuously in diverse cells under both anaerobic and aerobic conditions. Further, lactate produced at sites with high rates of glycolysis and glycogenolysis can be shuttled to adjacent or remote sites including heart or skeletal muscles where the lactate can be used as a gluconeogenic precursor or substrate for oxidation. The hypothesis was proposed 1985 by George Brooks of the University of California at Berkeley.
Dicarboxylic aminoaciduria is a rare form of aminoaciduria which is an autosomal recessive disorder of urinary glutamate and aspartate due to genetic errors related to transport of these amino acids. Mutations resulting in a lack of expression of the SLC1A1 gene, a member of the solute carrier family, are found to cause development of dicarboxylic aminoaciduria in humans. SLC1A1 encodes for EAAT3 which is found in the neurons, intestine, kidney, lung, and heart. EAAT3 is part of a family of high affinity glutamate transporters which transport both glutamate and aspartate across the plasma membrane.

The proton-coupled folate transporter is a protein that in humans is encoded by the SLC46A1 gene. The major physiological roles of PCFTs are in mediating the intestinal absorption of folate, and its delivery to the central nervous system.
References
- 1 2 3 4 5 Sivaprakasam S, Bhutia YD, Yang S, Ganapathy V (December 2017). "Short-Chain Fatty Acid Transporters: Role in Colonic Homeostasis". Comprehensive Physiology. 8 (1): 299–314. doi:10.1002/cphy.c170014. ISBN 9780470650714. PMC 6019286 . PMID 29357130.
- 1 2 3 Felmlee MA, Morse BL, Morris ME (January 2021). "γ-Hydroxybutyric Acid: Pharmacokinetics, Pharmacodynamics, and Toxicology". The AAPS Journal. 23 (1): 22. doi:10.1208/s12248-020-00543-z. PMC 8098080 . PMID 33417072.
- 1 2 Felmlee MA, Jones RS, Rodriguez-Cruz V, Follman KE, Morris ME (April 2020). "Monocarboxylate Transporters (SLC16): Function, Regulation, and Role in Health and Disease". Pharmacological Reviews. 72 (2): 466–485. doi:10.1124/pr.119.018762. PMC 7062045 . PMID 32144120.
- ↑ Song W, Li D, Tao L, Luo Q, Chen L (January 2020). "Solute carrier transporters: the metabolic gatekeepers of immune cells". Acta Pharmaceutica Sinica. B. 10 (1): 61–78. doi:10.1016/j.apsb.2019.12.006. PMC 6977534 . PMID 31993307.
- 1 2 3 Gopal E, Umapathy NS, Martin PM, Ananth S, Gnana-Prakasam JP, Becker H, Wagner CA, Ganapathy V, Prasad PD (November 2007). "Cloning and functional characterization of human SMCT2 (SLC5A12) and expression pattern of the transporter in kidney". Biochimica et Biophysica Acta (BBA) - Biomembranes. 1768 (11): 2690–7. doi:10.1016/j.bbamem.2007.06.031. PMC 2703486 . PMID 17692818.
- ↑ "UniProt".
- 1 2 3 4 Iwanaga T, Kishimoto A (2015). "Cellular distributions of monocarboxylate transporters: a review". Biomedical Research (Tokyo, Japan). 36 (5): 279–301. doi: 10.2220/biomedres.36.279 . PMID 26522146.
- 1 2 3 4 Ganapathy V, Thangaraju M, Gopal E, Martin PM, Itagaki S, Miyauchi S, Prasad PD (2008). "Sodium-coupled monocarboxylate transporters in normal tissues and in cancer". The AAPS Journal. 10 (1): 193–9. doi:10.1208/s12248-008-9022-y. PMC 2751467 . PMID 18446519.
- 1 2 Elangovan S, Pathania R, Ramachandran S, Ananth S, Padia RN, Srinivas SR, Babu E, Hawthorn L, Schoenlein PV, Boettger T, Smith SB, Prasad PD, Ganapathy V, Thangaraju M (October 2013). "Molecular mechanism of SLC5A8 inactivation in breast cancer". Molecular and Cellular Biology. 33 (19): 3920–35. doi:10.1128/MCB.01702-12. PMC 3811868 . PMID 23918800.
- 1 2 Kimura I, Ichimura A, Ohue-Kitano R, Igarashi M (January 2020). "Free Fatty Acid Receptors in Health and Disease". Physiological Reviews. 100 (1): 171–210. doi: 10.1152/physrev.00041.2018 . PMID 31487233. S2CID 201845937.
- 1 2 Cosín-Roger J, Ortiz-Masia D, Barrachina MD, Calatayud S (October 2020). "Metabolite Sensing GPCRs: Promising Therapeutic Targets for Cancer Treatment?". Cells. 9 (11): 2345. doi: 10.3390/cells9112345 . PMC 7690732 . PMID 33113952.
- 1 2 3 Martin PM, Dun Y, Mysona B, Ananth S, Roon P, Smith SB, Ganapathy V (July 2007). "Expression of the sodium-coupled monocarboxylate transporters SMCT1 (SLC5A8) and SMCT2 (SLC5A12) in retina". Investigative Ophthalmology & Visual Science. 48 (7): 3356–63. doi:10.1167/iovs.06-0888. PMID 17591909.
- 1 2 3 4 5 6 Srinivas SR, Gopal E, Zhuang L, Itagaki S, Martin PM, Fei YJ, Ganapathy V, Prasad PD (December 2005). "Cloning and functional identification of slc5a12 as a sodium-coupled low-affinity transporter for monocarboxylates (SMCT2)". The Biochemical Journal. 392 (Pt 3): 655–64. doi:10.1042/BJ20050927. PMC 1316307 . PMID 16104846.
- 1 2 Bongarzone S, Barbon E, Ferocino A, Alsulaimani L, Dunn J, Kim J, Sunassee K, Gee A (2020). "Imaging niacin trafficking with positron emission tomography reveals in vivo monocarboxylate transporter distribution". Nuclear Medicine and Biology. 88–89: 24–33. doi:10.1016/j.nucmedbio.2020.07.002. PMC 7599079 . PMID 32683248.
- ↑ Teramae H, Yoshikawa T, Inoue R, Ushida K, Takebe K, Nio-Kobayashi J, Iwanaga T (August 2010). "The cellular expression of SMCT2 and its comparison with other transporters for monocarboxylates in the mouse digestive tract". Biomedical Research (Tokyo, Japan). 31 (4): 239–49. doi: 10.2220/biomedres.31.239 . PMID 20834181.
- ↑ Wuerch E, Urgoiti GR, Yong VW (July 2023). "The Promise of Niacin in Neurology". Neurotherapeutics. 20 (4): 1037–1054. doi:10.1007/s13311-023-01376-2. PMC 10457276 . PMID 37084148.
- 1 2 Frank H, Gröger N, Diener M, Becker C, Braun T, Boettger T (September 2008). "Lactaturia and loss of sodium-dependent lactate uptake in the colon of SLC5A8-deficient mice". The Journal of Biological Chemistry. 283 (36): 24729–37. doi: 10.1074/jbc.M802681200 . PMC 3259809 . PMID 18562324.
- ↑ Thangaraju M, Ananth S, Martin PM, Roon P, Smith SB, Sterneck E, Prasad PD, Ganapathy V (September 2006). "c/ebpdelta Null mouse as a model for the double knock-out of slc5a8 and slc5a12 in kidney". The Journal of Biological Chemistry. 281 (37): 26769–73. doi: 10.1074/jbc.C600189200 . PMID 16873376.
- ↑ Gao H, A L, Huang X, Chen X, Xu H (May 2021). "Müller Glia-Mediated Retinal Regeneration". Molecular Neurobiology. 58 (5): 2342–2361. doi:10.1007/s12035-020-02274-w. PMID 33417229. S2CID 231192160.
- ↑ Juel C (November 2001). "Current aspects of lactate exchange: lactate/H+ transport in human skeletal muscle". European Journal of Applied Physiology. 86 (1): 12–6. doi:10.1007/s004210100517. PMID 11820315. S2CID 22025637.