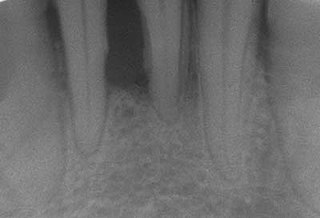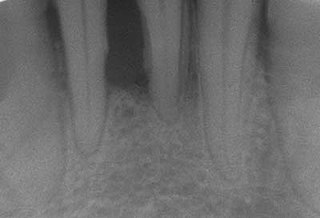
Periodontal disease, also known as gum disease, is a set of inflammatory conditions affecting the tissues surrounding the teeth. In its early stage, called gingivitis, the gums become swollen and red and may bleed. It is considered the main cause of tooth loss for adults worldwide. In its more serious form, called periodontitis, the gums can pull away from the tooth, bone can be lost, and the teeth may loosen or fall out. Halitosis may also occur.

Toothache, also known as dental pain or tooth pain, is pain in the teeth or their supporting structures, caused by dental diseases or pain referred to the teeth by non-dental diseases. When severe it may impact sleep, eating, and other daily activities.

Aphthous stomatitis, or recurrent aphthous stomatitis (RAS), is a common condition characterized by the repeated formation of benign and non-contagious mouth ulcers (aphthae) in otherwise healthy individuals. The informal term canker sore is also used, mainly in North America, although it may also refer to other types of mouth ulcers. The cause is not completely understood but involves a T cell-mediated immune response triggered by a variety of factors which may include nutritional deficiencies, local trauma, stress, hormonal influences, allergies, genetic predisposition, certain foods, dehydration, some food additives, or some hygienic chemical additives like SDS.

Stomatitis is inflammation of the mouth and lips. It refers to any inflammatory process affecting the mucous membranes of the mouth and lips, with or without oral ulceration.
Periodontology or periodontics is the specialty of dentistry that studies supporting structures of teeth, as well as diseases and conditions that affect them. The supporting tissues are known as the periodontium, which includes the gingiva (gums), alveolar bone, cementum, and the periodontal ligament. A periodontist is a dentist that specializes in the prevention, diagnosis and treatment of periodontal disease and in the placement of dental implants.
Dental plaque is a biofilm of microorganisms that grows on surfaces within the mouth. It is a sticky colorless deposit at first, but when it forms tartar, it is often brown or pale yellow. It is commonly found between the teeth, on the front of teeth, behind teeth, on chewing surfaces, along the gumline (supragingival), or below the gumline cervical margins (subgingival). Dental plaque is also known as microbial plaque, oral biofilm, dental biofilm, dental plaque biofilm or bacterial plaque biofilm. Bacterial plaque is one of the major causes for dental decay and gum disease.

Noma is a rapidly progressive and often fatal gangrenous infection of the mouth and face. Noma usually begins as an ulcer on gums and rapidly spreads into the jawbone, cheek, and soft tissues of the face. This is followed by death of the facial tissues and fatal sepsis. Survivors are left with severe facial disfigurement and impairments in breathing, swallowing, speaking and vision. In 2023 noma was added to the World Health Organization's list of neglected tropical diseases.

Pericoronitis is inflammation of the soft tissues surrounding the crown of a partially erupted tooth, including the gingiva (gums) and the dental follicle. The soft tissue covering a partially erupted tooth is known as an operculum, an area which can be difficult to access with normal oral hygiene methods. The hyponym operculitis technically refers to inflammation of the operculum alone.

Veterinary dentistry is the field of dentistry applied to the care of animals. It is the art and science of prevention, diagnosis, and treatment of conditions, diseases, and disorders of the oral cavity, the maxillofacial region, and its associated structures as it relates to animals.
Desquamative gingivitis is an erythematous (red), desquamatous (shedding) and ulcerated appearance of the gums. It is a descriptive term and can be caused by several different disorders.
Bleeding on probing (BoP) which is also known as bleeding gums or gingival bleeding is a term used by dentists and dental hygienists when referring to bleeding that is induced by gentle manipulation of the tissue at the depth of the gingival sulcus, or interface between the gingiva and a tooth. BoP is a sign of periodontal inflammation and indicates some sort of destruction and erosion to the lining of the sulcus or the ulceration of sulcular epithelium. The blood comes from lamina propria after the ulceration of the lining. BoP seems to be correlated with Periodontal Inflamed Surface Area (PISA).

Scaling and root planing, also known as conventional periodontal therapy, non-surgical periodontal therapy or deep cleaning, is a procedure involving removal of dental plaque and calculus and then smoothing, or planing, of the (exposed) surfaces of the roots, removing cementum or dentine that is impregnated with calculus, toxins, or microorganisms, the agents that cause inflammation. It is a part of non-surgical periodontal therapy. This helps to establish a periodontium that is in remission of periodontal disease. Periodontal scalers and periodontal curettes are some of the tools involved.
Oral and maxillofacial pathology refers to the diseases of the mouth, jaws and related structures such as salivary glands, temporomandibular joints, facial muscles and perioral skin. The mouth is an important organ with many different functions. It is also prone to a variety of medical and dental disorders.

Gingivitis is a non-destructive disease that causes inflammation of the gums; ulitis is an alternative term. The most common form of gingivitis, and the most common form of periodontal disease overall, is in response to bacterial biofilms that are attached to tooth surfaces, termed plaque-induced gingivitis. Most forms of gingivitis are plaque-induced.

A periodontal abscess, is a localized collection of pus within the tissues of the periodontium. It is a type of dental abscess. A periodontal abscess occurs alongside a tooth, and is different from the more common periapical abscess, which represents the spread of infection from a dead tooth. To reflect this, sometimes the term "lateral (periodontal) abscess" is used. In contrast to a periapical abscess, periodontal abscesses are usually associated with a vital (living) tooth. Abscesses of the periodontium are acute bacterial infections classified primarily by location.
Chronic periodontitis is one of the seven categories of periodontitis as defined by the American Academy of Periodontology 1999 classification system. Chronic periodontitis is a common disease of the oral cavity consisting of chronic inflammation of the periodontal tissues that is caused by the accumulation of profuse amounts of dental plaque. Periodontitis initially begins as gingivitis and can progress onto chronic and subsequent aggressive periodontitis according to the 1999 classification.

Necrotizing periodontal diseases is one of the three categories of periodontitis as defined by the American Academy of Periodontology/European Federation of Periodontology 2017 World Workshop classification system.
In dentistry, numerous types of classification schemes have been developed to describe the teeth and gum tissue in a way that categorizes various defects. All of these classification schemes combine to provide the periodontal diagnosis of the aforementioned tissues in their various states of health and disease.
Oral manifestations of systematic disease are signs and symptoms of disease occurring elsewhere in the body detected in the oral cavity and oral secretions. High blood sugar can be detected by sampling saliva. Saliva sampling may be a non-invasive way to detect changes in the gut microbiome and changes in systemic disease. Another example is tertiary syphilis, where changes to teeth can occur. Syphilis infection can be associated with longitudinal furrows of the tongue.