Related Research Articles

Bacterial vaginosis (BV) is an infection of the vagina caused by excessive growth of bacteria. Common symptoms include increased vaginal discharge that often smells like fish. The discharge is usually white or gray in color. Burning with urination may occur. Itching is uncommon. Occasionally, there may be no symptoms. Having BV approximately doubles the risk of infection by a number of sexually transmitted infections, including HIV/AIDS. It also increases the risk of early delivery among pregnant women.

Pelvic inflammatory disease, also known as pelvic inflammatory disorder (PID), is an infection of the upper part of the female reproductive system, namely the uterus, fallopian tubes, and ovaries, and inside of the pelvis. Often, there may be no symptoms. Signs and symptoms, when present, may include lower abdominal pain, vaginal discharge, fever, burning with urination, pain with sex, bleeding after sex, or irregular menstruation. Untreated PID can result in long-term complications including infertility, ectopic pregnancy, chronic pelvic pain, and cancer.
Nongonococcal urethritis (NGU) is inflammation of the urethra that is not caused by gonorrheal infection.
Gardnerella vaginalis is a species of Gram-variable-staining facultative anaerobic bacteria. The organisms are small non-spore-forming, nonmotile coccobacilli.
Vaginitis, also known as vulvovaginitis, is inflammation of the vagina and vulva. Symptoms may include itching, burning, pain, discharge, and a bad smell. Certain types of vaginitis may result in complications during pregnancy.
Mycoplasma hominis is a species of bacteria in the genus Mycoplasma. M. hominis has the ability to penetrate the interior of human cells. Along with ureaplasmas, mycoplasmas are the smallest free-living organisms known.

Ureaplasma urealyticum is a bacterium belonging to the genus Ureaplasma and the family Mycoplasmataceae in the order Mycoplasmatales. This family consists of the genera Mycoplasma and Ureaplasma. Its type strain is T960. There are two known biovars of this species; T960 and 27. These strains of bacteria are commonly found as commensals in the urogenital tracts of human beings, but overgrowth can lead to infections that cause the patient discomfort. Unlike most bacteria, Ureaplasma urealyticum lacks a cell wall making it unique in physiology and medical treatment.

Mycoplasmataceae is a family of bacteria in the order Mycoplasmatales. This family consists of the genera Mycoplasma and Ureaplasma.

An opportunistic infection is an infection caused by pathogens that take advantage of an opportunity not normally available. These opportunities can stem from a variety of sources, such as a weakened immune system, an altered microbiome, or breached integumentary barriers. Many of these pathogens do not necessarily cause disease in a healthy host that has a non-compromised immune system, and can, in some cases, act as commensals until the balance of the immune system is disrupted. Opportunistic infections can also be attributed to pathogens which cause mild illness in healthy individuals but lead to more serious illness when given the opportunity to take advantage of an immunocompromised host.
Atopobium is a genus of Actinomycetota, in the family Coriobacteriaceae. Atopobium species are anaerobic, Gram-positive rod-shaped or elliptical bacteria found as single elements or in pairs or short chains.
Pichia kudriavzevii is a budding yeast involved in chocolate production. P. kudriavzevii is an emerging fungal nosocomial pathogen primarily found in the immunocompromised and those with hematological malignancies. It has natural resistance to fluconazole, a standard antifungal agent. It is most often found in patients who have had prior fluconazole exposure, sparking debate and conflicting evidence as to whether fluconazole should be used prophylactically. Mortality due to P. kudriavzevii fungemia is much higher than the more common C. albicans. Other Candida species that also fit this profile are C. parapsilosis, C. glabrata, C. tropicalis, C. guillermondii and C. rugosa.
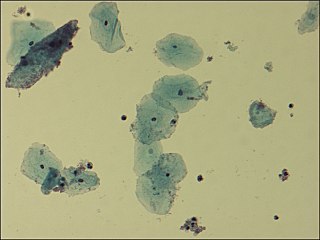
The Nugent Score is a Gram stain scoring system for vaginal swabs to diagnose bacterial vaginosis (BV). The Nugent score is calculated by assessing for the presence of large Gram-positive rods, small Gram-variable rods, and curved Gram-variable rods. A score of 7 to 10 is consistent with bacterial vaginosis without culture. The Nugent Score is now rarely used by physicians due to the time it takes to read the slides and requires the use of a trained microscopist. Bacterial vaginosis diagnosis is done by evaluating the pH, the presences of Lactobacillus spp. versus a mixed flora consisting of Gardnerella vaginalis, Bacteroides spp, Mobiluncus spp, and Mycoplasma hominis. The Amsel Criteria for bacterial vaginosis includes pH, evaluating the presence of clue cells, white discharge and an odor of amines after mixing with KOH.

Vaginal flora, vaginal microbiota or vaginal microbiome are the microorganisms that colonize the vagina. They were discovered by the German gynecologist Albert Döderlein in 1892 and are part of the overall human flora. The amount and type of bacteria present have significant implications for an individual's overall health. The primary colonizing bacteria of a healthy individual are of the genus Lactobacillus, such as L. crispatus, and the lactic acid they produce is thought to protect against infection by pathogenic species.
Prevotella is a genus of Gram-negative bacteria.
Ureaplasma parvum is a species of Ureaplasma, a genus of bacteria belonging to the family Mycoplasmataceae. In Indonesia, ureaplasma parvum is most commonly contracted through contact with public toilets.
Lactobacillus iners is a species in the genus Lactobacillus. It is a Gram-positive, catalase-negative, facultatively anaerobic rod-shaped bacterium. Lactobacillus iners is a normal inhabitant of the lower reproductive tract in healthy women.
Fannyhessea vaginae is a species of bacteria in the family Atopobiaceae. It is a facultative anaerobic, Gram-positive rod-shaped or elliptical coccobacillus found as single elements or in pairs or short chains. It is typically isolated from 80% of women with bacterial vaginosis and it is implicated in treatment failures. Invasive infections such as bacteremia have been reported.
Lactobacillus crispatus is a common, rod-shaped species of genus Lactobacillus and is a hydrogen peroxide (H2O2) producing beneficial microbiota species located in both the vagina, through vaginal discharge, and the vertebrate gastrointestinal tract. The strain CTV-05 is used as a probiotic that can be used by premenopausal and postmenopausal women that experience recurrent urinary tract infections. It is being evaluated specifically for the prevention and treatment of bacterial vaginosis, which is characterized by the absence of Lactobacillus flora necessary to protect the host from infection.
The vaginal flora in pregnancy, or vaginal microbiota in pregnancy, is different from the vaginal flora before sexual maturity, during reproductive years, and after menopause. A description of the vaginal flora of pregnant women who are immunocompromised is not covered in this article. The composition of the vaginal flora significantly differs in pregnancy. Bacteria or viruses that are infectious most often have no symptoms.
References
- ↑ Amaya-Guio, Jairo; Martinez-Velasquez, Mercy Yolima; Viveros-Carreño, David Andres; Sierra-Barrios, Eloisa Mercedes; Grillo-Ardila, Carlos F; Amaya-Guio, Jairo (2015). Amaya-Guio, Jairo (ed.). "Antibiotic treatment for the sexual partners of women with bacterial vaginosis". Protocols. doi:10.1002/14651858.CD011701.
- ↑ "Bacterial Vaginosis (BV): Condition Information". National Institute of Child Health and Human Development. 2013-05-21. Retrieved 3 March 2015.
- ↑ Nardis, C.; Mastromarino, P.; Mosca, L. (September 2013). "Vaginal microbiota and viral sexually transmitted diseases". Annali di Igiene. 25 (5): 443–56. doi:10.7416/ai.2013.1946. PMID 24048183.
- 1 2 3 4 5 6 7 Clark, Natalie; Tal, Reshef; Sharma, Harsha; Segars, James (2014). "Microbiota and Pelvic Inflammatory Disease". Seminars in Reproductive Medicine. 32 (1): 043–049. doi:10.1055/s-0033-1361822. ISSN 1526-8004. PMC 4148456 . PMID 24390920.
- ↑ "What are the symptoms of bacterial vaginosis?". National Institute of Child Health and Human Development. 2013-05-21. Retrieved 3 March 2015.
- 1 2 3 4 Larsen, Bryan; Hwang, Joseph (2010). "Mycoplasma, Ureaplasma, and Adverse Pregnancy Outcomes: A Fresh Look". Infectious Diseases in Obstetrics and Gynecology. 2010: 1–7. doi: 10.1155/2010/521921 . ISSN 1064-7449. PMC 2913664 . PMID 20706675.
- ↑ Kenyon, C; Colebunders, R; Crucitti, T (December 2013). "The global epidemiology of bacterial vaginosis: a systematic review". American Journal of Obstetrics and Gynecology. 209 (6): 505–23. doi:10.1016/j.ajog.2013.05.006. PMID 23659989.
- ↑ "What are the treatments for bacterial vaginosis (BV)?". National Institute of Child Health and Human Development. 2013-07-15. Retrieved 9 May 2015.
- 1 2 3 4 5 6 Mastromarino, Paola; Vitali, Beatrice; Mosca, Luciana (2013). "Bacterial vaginosis: a review on clinical trials with probiotics" (PDF). New Microbiologica. 36 (3): 229–238. PMID 23912864.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 Africa, Charlene; Nel, Janske; Stemmet, Megan (2014). "Anaerobes and Bacterial Vaginosis in Pregnancy: Virulence Factors Contributing to Vaginal Colonisation". International Journal of Environmental Research and Public Health. 11 (7): 6979–7000. doi: 10.3390/ijerph110706979 . ISSN 1660-4601. PMC 4113856 . PMID 25014248.
- ↑ Mastromarino, Paola; Vitali, Beatrice; Mosca, Luciana (2013). "Bacterial vaginosis: a review on clinical trials with probiotics" (PDF). New Microbiologica. 36 (3): 229–238. PMID 23912864.
- ↑ Knoester, M.; Lashley, L. E. E. L. O.; Wessels, E.; Oepkes, D.; Kuijper, E. J. (2011). "First Report of Atopobium vaginae Bacteremia with Fetal Loss after Chorionic Villus Sampling". Journal of Clinical Microbiology. 49 (4): 1684–1686. doi:10.1128/JCM.01655-10. ISSN 0095-1137. PMC 3122803 . PMID 21289141.
- ↑ Rabe, Lorna K.; Winterscheid, Karen K.; Hillier, Sharon L. (1988). "Association of viridans group streptococci from pregnant women with bacterial vaginosis and upper genital tract infection". Journal of Clinical Microbiology. 26 (6): 1156–1160. doi:10.1128/jcm.26.6.1156-1160.1988. ISSN 0095-1137. PMC 266553 . PMID 2454943.
- ↑ Spiegel, Carol A. (1991). "Bacterial Vaginosis". Clinical Microbiology Reviews. 4 (4): 485–502. doi: 10.1128/CMR.4.4.485 . ISSN 0893-8512. PMC 358214 . PMID 1747864.