Streptococcus is a genus of gram-positive coccus or spherical bacteria that belongs to the family Streptococcaceae, within the order Lactobacillales, in the phylum Bacillota. Cell division in streptococci occurs along a single axis, thus when growing they tend to form pairs or chains, which may appear bent or twisted. This differs from staphylococci, which divide along multiple axes, thereby generating irregular, grape-like clusters of cells. Most streptococci are oxidase-negative and catalase-negative, and many are facultative anaerobes.

Group A streptococcal infections are a number of infections with Streptococcus pyogenes, a group A streptococcus (GAS). S. pyogenes is a species of beta-hemolytic Gram-positive bacteria that is responsible for a wide range of infections that are mostly common and fairly mild. If the bacteria enter the bloodstream an infection can become severe and life-threatening, and is called an invasive GAS (iGAS).

Streptococcus pyogenes is a species of Gram-positive, aerotolerant bacteria in the genus Streptococcus. These bacteria are extracellular, and made up of non-motile and non-sporing cocci that tend to link in chains. They are clinically important for humans, as they are an infrequent, but usually pathogenic, part of the skin microbiota that can cause Group A streptococcal infection. S. pyogenes is the predominant species harboring the Lancefield group A antigen, and is often called group A Streptococcus (GAS). However, both Streptococcus dysgalactiae and the Streptococcus anginosus group can possess group A antigen as well. Group A streptococci, when grown on blood agar, typically produce small (2–3 mm) zones of beta-hemolysis, a complete destruction of red blood cells. The name group A (beta-hemolytic) Streptococcus is thus also used.

Scarlet fever, also known as scarlatina, is an infectious disease caused by Streptococcus pyogenes, a Group A streptococcus (GAS). It most commonly affects children between five and 15 years of age. The signs and symptoms include a sore throat, fever, headache, swollen lymph nodes, and a characteristic rash. The face is flushed and the rash is red and blanching. It typically feels like sandpaper and the tongue may be red and bumpy. The rash occurs as a result of capillary damage by exotoxins produced by S.pyogenes. On darker-pigmented skin the rash may be hard to discern.

Streptococcal pharyngitis, also known as streptococcal sore throat, is pharyngitis caused by Streptococcus pyogenes, a gram-positive, group A streptococcus. Common symptoms include fever, sore throat, red tonsils, and enlarged lymph nodes in the front of the neck. A headache and nausea or vomiting may also occur. Some develop a sandpaper-like rash which is known as scarlet fever. Symptoms typically begin one to three days after exposure and last seven to ten days.

Lemierre's syndrome is infectious thrombophlebitis of the internal jugular vein. It most often develops as a complication of a bacterial sore throat infection in young, otherwise healthy adults. The thrombophlebitis is a serious condition and may lead to further systemic complications such as bacteria in the blood or septic emboli.

Pharyngitis is inflammation of the back of the throat, known as the pharynx. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, difficulty swallowing, swollen lymph nodes, and a hoarse voice. Symptoms usually last 3–5 days, but can be longer depending on cause. Complications can include sinusitis and acute otitis media. Pharyngitis is a type of upper respiratory tract infection.

Sore throat, also known as throat pain, is pain or irritation of the throat. Usually, causes of sore throat include:

Rheumatic fever (RF) is an inflammatory disease that can involve the heart, joints, skin, and brain. The disease typically develops two to four weeks after a streptococcal throat infection. Signs and symptoms include fever, multiple painful joints, involuntary muscle movements, and occasionally a characteristic non-itchy rash known as erythema marginatum. The heart is involved in about half of the cases. Damage to the heart valves, known as rheumatic heart disease (RHD), usually occurs after repeated attacks but can sometimes occur after one. The damaged valves may result in heart failure, atrial fibrillation and infection of the valves.

An upper respiratory tract infection (URTI) is an illness caused by an acute infection, which involves the upper respiratory tract, including the nose, sinuses, pharynx, larynx or trachea. This commonly includes nasal obstruction, sore throat, tonsillitis, pharyngitis, laryngitis, sinusitis, otitis media, and the common cold. Most infections are viral in nature, and in other instances, the cause is bacterial. URTIs can also be fungal or helminthic in origin, but these are less common.

Tonsillitis is inflammation of the tonsils in the upper part of the throat. It can be acute or chronic. Acute tonsillitis typically has a rapid onset. Symptoms may include sore throat, fever, enlargement of the tonsils, trouble swallowing, and enlarged lymph nodes around the neck. Complications include peritonsillar abscess (Quinsy).

Peritonsillar abscess (PTA), also known as quinsy, is an accumulation of pus due to an infection behind the tonsil. Symptoms include fever, throat pain, trouble opening the mouth, and a change to the voice. Pain is usually worse on one side. Complications may include blockage of the airway or aspiration pneumonitis.
A complication in medicine, or medical complication, is an unfavorable result of a disease, health condition, or treatment. Complications may adversely affect the prognosis, or outcome, of a disease. Complications generally involve a worsening in the severity of the disease or the development of new signs, symptoms, or pathological changes that may become widespread throughout the body and affect other organ systems. Thus, complications may lead to the development of new diseases resulting from previously existing diseases. Complications may also arise as a result of various treatments.

Group B streptococcal infection, also known as Group B streptococcal disease or just Group B strep infection, is the infectious disease caused by the bacterium Streptococcus agalactiae, which is the most common human pathogen belonging to the group B of the Lancefield classification of streptococci—hence the group B stretococcal (GBS) infection nomenclature. Infection with GBS can cause serious illness and sometimes death, especially in newborns, the elderly, and people with compromised immune systems. The most severe form of group B streptococcal disease is neonatal meningitis in infants, which is frequently lethal and can cause permanent neuro-cognitive impairment.
Fusobacterium necrophorum is a species of bacteria responsible for Lemierre's syndrome. It has also been known to cause sinusitis, mastoiditis, and odontogenic infections.
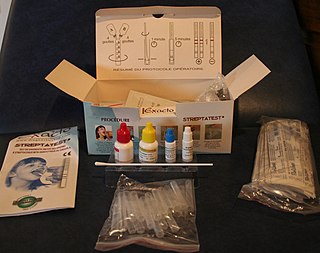
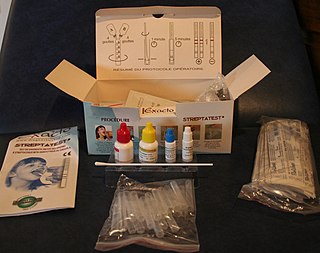
The rapid strep test (RST) is a rapid antigen detection test (RADT) that is widely used in clinics to assist in the diagnosis of bacterial pharyngitis caused by group A streptococci (GAS), sometimes termed strep throat. There are currently several types of rapid strep test in use, each employing a distinct technology. However, they all work by detecting the presence of GAS in the throat of a person by responding to GAS-specific antigens on a throat swab.

A throat culture is a laboratory diagnostic test that evaluates for the presence of a bacterial or fungal infection in the throat. A sample from the throat is collected by swabbing the throat and placing the sample into a special cup (culture) that allows infections to grow. If an organism grows, the culture is positive and the presence of an infection is confirmed. The type of infection is found using a microscope, chemical tests, or both. If no infection grows, the culture is negative. Common infectious organisms tested for by a throat culture include Candida albicans known for causing thrush and Group A streptococcus known for causing strep throat, scarlet fever, and rheumatic fever. Throat cultures are more sensitive than the rapid strep test (70%) for diagnosing strep throat, but are nearly equal in terms of specificity.
Perianal cellulitis, also known as perianitis or perianal streptococcal dermatitis, is a bacterial infection affecting the lower layers of the skin (cellulitis) around the anus. It presents as bright redness in the skin and can be accompanied by pain, difficulty defecating, itching, and bleeding. This disease is considered a complicated skin and soft tissue infection (cSSTI) because of the involvement of the deeper soft tissues.
Throat irritation can refer to a dry cough, a scratchy feeling at the back of the throat, a sensation of a lumpy feeling, something stuck at the back of the throat, or possibly a feeling of dust in the throat. The symptoms are unpleasant and usually temporary, but occasionally signifies a more serious health issue, such as laryngitis.
Anti-Deoxyribonuclease B titres are a quantitative measure of the presence of serologic antibodies obtained from patients suspected of having a recent group A (Beta-hemolytic) streptococcus bacteria infection, from Streptococcus pyogenes.